Dec. 22, 2023
Mayo Clinic is at the forefront of new technologies that improve care for people with medication-refractory epilepsy. Neurosurgeons have expertise with a range of options for managing intractable seizures.
"There are very few epilepsies that we can't treat," says Jamie J. Van Gompel, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota.
Approximately one-third of individuals with epilepsy have medication-refractory seizures and might benefit from other therapies if epileptogenic lesions are identified. Mayo Clinic neuroradiologists are leaders in the development and use of sophisticated imaging, including:
- Morphometric analysis program (MAP) imaging.
- High-frequency oscillation density mapping.
- 7T MRI.
- Positron emission tomography (PET) MRI.
- Single-photon emission computerized tomography (SPECT) coregistered to MRI (SISCOM) and statistical ictal SPECT coregistered to MRI (STATISCOM).
"We continue to push the limits of what we can do with technology," says Steven A. Messina, M.D., a neuroradiologist at Mayo Clinic's campus in Minnesota. "Our goal is to identify every possible candidate for epilepsy therapy, to potentially improve their chances of seizure freedom."
"Polyneurostimulation can be considered when an individual's response to vagus nerve stimulation is suboptimal."
Treatment options include several types of neurostimulation and ablative therapies. "Our goal is to be as minimally invasive as possible, so we can treat the epilepsy while preserving function," says Kai J. Miller, M.D., Ph.D., a neurosurgeon at Mayo Clinic's campus in Minnesota.
Cutting-edge neurostimulation
Mayo Clinic neurosurgeons have extensive experience with various methods of neurostimulation for the treatment of epilepsy. They include:
- Vagus nerve stimulation, which uses a device implanted under the skin in the chest to send regular, mild pulses of electrical energy to the brain via the vagus nerve.
- Deep brain stimulation, which delivers controlled pulses to a target in the brain that is part of a circuit involved in seizures.
- Responsive neurostimulation, which monitors brain waves to detect the likely onset of seizures and stop them before they cause clinical symptoms.
- Polyneurostimulation, which combines vagus nerve stimulation with deep brain stimulation or responsive neurostimulation.
"Polyneurostimulation can be considered when an individual's response to vagus nerve stimulation is suboptimal," says Brin E. Freund, M.D., a neurologist at Mayo Clinic in Jacksonville, Florida. "Some patients see an additive response to multiple neuromodulators — similar to how we would use multiple medications."
A retrospective study of patients who had polyneurostimulation at Mayo Clinic demonstrated the approach's safety and feasibility. Published in the May 2022 issue of World Neurosurgery and cited in the February 2023 issue of Neuromodulation, the study described the case of a 44-year-old patient with drug-resistant genetic generalized epilepsy. She was not a candidate for surgical resection, had a suboptimal response to vagus nerve stimulation placement and required better seizure control.
The addition of deep brain stimulation to vagus nerve stimulation led to seizure freedom. "Her driving privileges were reinstated, and she married her partner and obtained gainful employment," Dr. Freund says.
Neurostimulation sometimes involves complex electrode placements. Each of Mayo Clinic's main campuses has a robotic system that can increase the accuracy and efficiency of these procedures.
"The robotic system allows us to tackle more-challenging cases of epilepsy," says Jonathon J. Parker, M.D., Ph.D., a neurosurgeon at Mayo Clinic in Phoenix/Scottsdale, Arizona.
Additional methods of neurostimulation include:
- Chronic subthreshold cortical stimulation, which provides continuous electrical impulses to an area of seizure onset to suppress the generation of the abnormal seizure discharge.
- Transcranial magnetic stimulation, which uses an electromagnetic coil placed against the scalp to stimulate nerve cells in the brain.
"We are committed to innovation to serve the needs of our patients and to developing methods for selecting the best type of stimulation to suppress seizures," Dr. Parker says.
Ablative therapies
As an early adopter of ablative technologies, Mayo Clinic has experience applying these minimally invasive approaches to disable seizure origin sites.
Tratamiento de invasión mínima
Tratamiento de invasión mínima
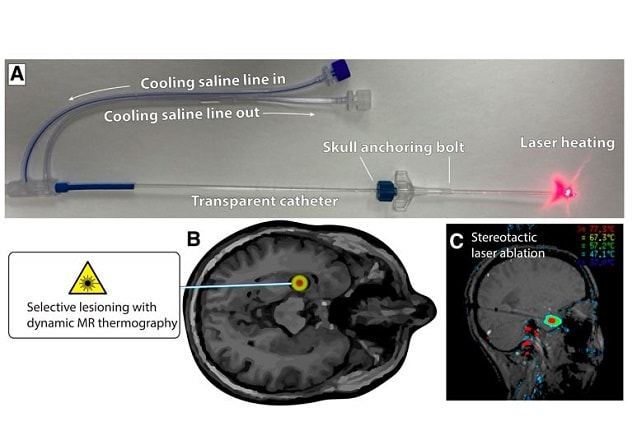
En la ilustración, se muestra la terapia térmica intersticial con láser. A. Se coloca un perno para sujetar el cráneo a través de un pequeño orificio en este. A través del orificio se introduce un catéter transparente y se lo lleva hasta el objetivo en el cerebro. B. De forma selectiva, se producen lesiones en el cerebro con la ayuda de las imágenes por resonancia magnética y se calienta solo el objetivo profundo, sin dañar el tejido cerebral que se encuentra alrededor. C. Las secuencias especializadas de las imágenes por resonancia magnética generan mapas de la temperatura en tiempo real, que los médicos vigilan atentamente durante el procedimiento.
MRI-guided laser interstitial thermal therapy (LITT) avoids the neurological, neuropsychological and procedure-related complications of open surgery. The procedure provides real-time feedback on the tissue being ablated.
"That allows us to maximize the removal of seizure-generating tissue while avoiding damage to eloquent tissue," says Richard S. Zimmerman, M.D., a neurosurgeon at Mayo Clinic's campus in Arizona. For treatments involving multiple trajectories, the robotic system can be used to precisely contour laser ablations.
LITT is most commonly used to treat deep-seated lesions in temporal lobe epilepsy. Other epileptic conditions treated with LITT include:
- Encephaloceles.
- Epileptogenic tissue aberrancies, such as focal cortical dysplasia, gray matter heterotopia and cortical tubers.
- Epileptogenic brain tumors, such as neuroglial tumors and gangliogliomas.
- Hypothalamic hamartomas.
Mayo Clinic researchers are investigating the potential of another ablative therapy — MRI-guided focused ultrasound — to treat seizure origin zones. "The focused ultrasound energy ablates highly selected areas that we can select on imaging — disrupting the epilepsy network without surgical resection of the lesion," Dr. Van Gompel says. "Our hope is eventually to make many of these patients seizure-free without ever having to make an incision."
To that end, Mayo Clinic embraces new technologies. "Our highly trained neurosurgeons, neuroradiologists and epileptologists are willing to try new treatment modalities," Dr. Freund says. "We are working to expand our armamentarium in the treatment of patients who are drug resistant but not candidates for surgical resection."
For more information
Freund B, et al. Dual-device neuromodulation in epilepsy. World Neurosurgery. 2022;161:e596.
Freund BE, et al. Dual-device neuromodulation can be effective in drug-resistant generalized epilepsies. Neuromodulation. 2023;26:480.
Refer a patient to Mayo Clinic.