Dec. 21, 2021
Mayo Clinic is exploring whether a protein might provide an adjunct therapy to help people with cervical spondylotic myelopathy regain function after surgery. The laboratory research could potentially improve outcomes for individuals with this common and debilitating condition.
"Since there is no adjunct treatment right now, all we can do after spinal decompression surgery is hope that patients achieve whatever progress improvement they can. An adjunct therapy is definitely needed," says Kingsley Abode-Iyamah, M.D., a neurosurgeon at Mayo Clinic in Jacksonville, Florida. "We're examining whether a particular protein can help the spinal cord to recover from the injuries caused by chronic compression."
Compresión de la médula espinal
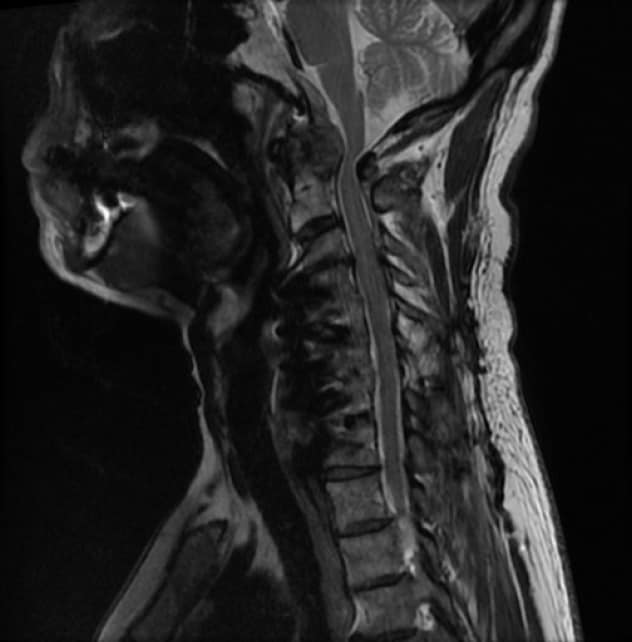
Compresión de la médula espinal
La resonancia magnética sagital muestra el retorcimiento y la compresión de la médula espinal en la unión occipitocervical, con el cambio de señal del cordón asociado que representa un daño continuo en la médula espinal.
Resolución postoperatoria

Resolución postoperatoria
La resonancia magnética después de la descompresión muestra la resolución de los cambios degenerativos que causaron compresión en la unión occipitocervical.
Cervical spondylotic myelopathy is the leading cause of spinal cord-related disability as people age. The condition can lead to gait instability, weakness, paresthesia, loss of dexterity in the upper extremities and urinary dysfunction. These signs and symptoms are caused by compression of the spinal cord from conditions such as disk degeneration, bulging or herniated disks, and spondylosis. After spinal decompression surgery, up to 25% of patients with cervical spondylotic myelopathy require re-operation for the recurrence of signs and symptoms.
Mayo Clinic's research builds on a discovery by Dr. Abode-Iyamah and colleagues that implicated a genetic mutation in the development and severity of cervical spondylotic myelopathy. Known as Val66Met polymorphism, the mutation is in the brain-derived neurotrophic factor gene — which has been implicated in several neurological and psychological conditions.
"Previous studies have shown that the polymorphism is more common in patients with cervical spondylotic myelopathy than in the general population," Dr. Abode-Iyamah says.
In the current laboratory studies, animal models of cervical spondylotic myelopathy receive a protein-based therapy delivered via nanoparticles. The models are then assessed to determine whether the therapy improves function.
The researchers are also comparing cervical spondylotic myelopathy outcomes for patients with and without the polymorphism. "We believe patients with the mutation may do worse," Dr. Abode-Iyamah says.
This type of work exemplifies Mayo Clinic's commitment to laboratory research that ultimately benefits patient care. Clinicians routinely work with laboratory scientists to promote innovation.
"The close collaboration and resources available not only to laboratory staff but also clinicians allow us to think outside the box and really concentrate on improving patient care," Dr. Abode-Iyamah says.