April 16, 2014
The apical variant of hypertrophic cardiomyopathy (HCM) accounts for approximately 25 percent of the total HCM population in Asians and less than 10 percent in non-Asians. It is an autosomal dominant genetic disease with variable phenotypic penetrance. Studies in Asian populations suggest that it has a more benign prognosis than other types of HCM. Data in non-Asian populations is limited, but small studies suggest that the prognostic implications of apical HCM may be more severe in this group than in affected Asian individuals.
Largest non-Asian clinical population to date
A review of the comprehensive Mayo Clinic HCM and echocardiographic databases was conducted by Kyle W. Klarich, M.D., cardiologist and director of the Cardiovascular Diseases Fellowship at Mayo Clinic in Rochester, Minn., and published in 2013 in the American Journal of Cardiology. She and her colleagues retrospectively identified 2,662 individuals with HCM evaluated at Mayo Clinic between June 1976 and September 2006. Of these individuals, 193 patients (7.3 percent) without confounding factors were classified as apical HCM, and follow-up was obtained in 187 of them (114 men, mean age 62 ± 19 years; 73 women, mean age 66 ± 16 years). Mean duration of follow-up was 94 ± 76 months.
Curvas de supervivencia de Kaplan-Meier
Curvas de supervivencia de Kaplan-Meier
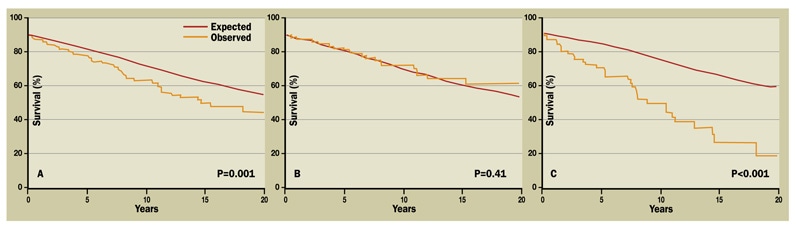
A. Supervivencia de 10 y 20 años en todos los pacientes. B. La supervivencia en hombres con miocardiopatía hipertrófica (MCH) apical fue equivalente a los controles de igual edad y sexo. C. La supervivencia en mujeres con MCH apical fue significativamente peor que los controles de igual edad y sexo. Reproducción con permiso de American Journal of Cardiology. 2013;111:1784.
There were 55 deaths; 21 had noncardiac causes, 27 were from unknown causes and 7 were of cardiac etiology. While Kaplan-Meier analysis demonstrated that the observed overall survival of this group of North American patients was significantly worse than expected, this finding was entirely due to excess mortality in women. Survival in men with apical HCM was almost identical to age-matched controls. Multivariate predictors of increased mortality included female sex, age at first visit, chronic atrial fibrillation and history of stroke.
"The increased mortality observed in women with apical HCM is likely due to older age at first visit and the presence of chronic atrial fibrillation. The mortality rate approaches what has been reported for other HCM phenotypes," says Dr. Klarich. "However, as with other cardiovascular diseases, we do not yet understand the role of hormonal and other sex-specific factors that may affect phenotypic onset, expression and progression of this disease."
Genetic testing for and analysis of sarcomeric mutations characteristic in HCM were not routinely performed in these patients, so mutational correlation could not be performed. While cardiac MRI is currently the preferred imaging modality for assessing both apical wall thickness and the presence of an apical pouch (although echocardiographic detection of apical pouch can be improved by contrast imaging) in these patients, this technology was introduced after the time frame included in this study and therefore not included in this analysis.
"Unfortunately, to date, genetic mutations in isolation are not reliable prognostic predictors," says Dr. Klarich. "As our understanding of the role of environmental and other genetic factors on mutational gene expression expands, we hope to better predict and improve outcomes for this group of patients."
This study suggests that apical HCM has different prognostic implications for affected women than affected men. The finding that the excess mortality in women is responsible for decreased survival in North Americans with apical HCM will help to focus future investigations.
For more information
Klarich KW, et al. Risk of death in long-term follow-up of patients with apical hypertrophic cardiomyopathy. American Journal of Cardiology. 2013;111:1784.