Overview
Vulvodynia (vul-voe-DIN-e-uh) is a type of long-term pain or discomfort around the outer part of the female genitals, called the vulva. It lasts at least three months and has no clear cause. The pain, burning or irritation linked with vulvodynia can make you so uncomfortable that sitting for a long time or having sex becomes unthinkable. The condition can last for months to years.
If you have symptoms of vulvodynia, don't let embarrassment or a lack of visible signs stop you from talking with your gynecologist or another healthcare professional. Treatments can ease your discomfort. And your care team might be able to find a cause for your pain. So, it's key to get a medical exam.
Symptoms
Vulva
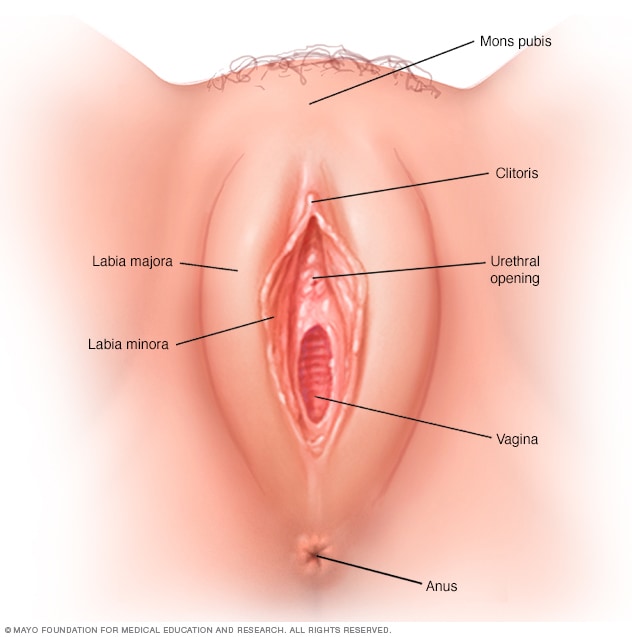
Vulva
The vulva is the outer part of the female genitalia, including the labia majora, labia minora and clitoris.
The main vulvodynia symptom is pain in the vulva, which includes the opening of the vagina. The pain often is described as:
- Burning.
- Irritation.
- Stinging.
- Rawness.
- Soreness.
- Sharp or knife-like pain.
You also may feel aching, throbbing and swelling.
How often the symptoms happen and where exactly they're felt varies from person to person. Your pain might be constant, or it may come and go. It might flare up only when the vulva is touched. You might feel the pain throughout your entire vulva. This is called generalized vulvodynia. Or the pain may flare up in a certain area, such as the tissue surrounding the opening of the vagina, called the vestibule. This is known as localized vulvodynia, and it's more common than the generalized kind.
The tissue of the vulva might look slightly inflamed or swollen. More often, your vulva doesn't look different than usual.
When to see a doctor
If you have pain in your vulva, talk with your gynecologist or another member of your healthcare team. If you don't have a gynecologist, you might be referred to one. A healthcare professional needs to find out if your pain has a treatable cause that's different from vulvodynia, such as:
- An active infection from yeast or bacteria.
- A sexually transmitted disease such as herpes.
- An inflammatory skin condition.
- Vulvar growths.
- Genitourinary syndrome of menopause.
Some people who don't realize they have vulvodynia try to ease their symptoms by using yeast infection treatments without a prescription. But it's key to get a checkup, so a member of your healthcare team can give you an exam and recommend the right treatment for you.
Causes
Experts don't know what causes vulvodynia. Factors that might play a role include:
- Injury to or irritation of the nerves of the vulva.
- Past infections of the vagina.
- Painful swelling called inflammation that affects the vulva.
- Some genetic conditions.
- Allergies.
- Hormonal changes.
- Muscle spasm or weakness in the pelvic floor, which supports the uterus, bladder and bowel.
Complications
Without treatment, vulvodynia can affect mental health, relationships and other aspects of your life.
The condition is linked with anxiety and depression. It's also tied to less sexual desire, arousal and enjoyment. Fear of having painful sex can cause spasms in the muscles around the vagina, a condition called vaginismus. Intimacy issues such as these lead many people with vulvodynia to say they feel shame, lower self-esteem, negative about body image and lacking as a sexual partner.
The pain and other symptoms of vulvodynia might make it harder to keep up with work. You may feel less social too. And you may have trouble getting quality sleep.
Sept. 01, 2023