Overview
Male reproductive system
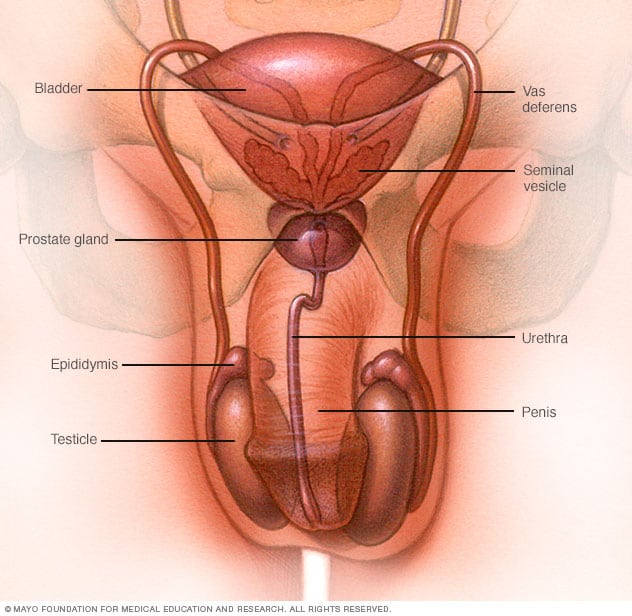
Male reproductive system
The male reproductive system makes, stores and moves sperm. Testicles produce sperm. Fluid from the seminal vesicles and prostate gland mixes with sperm to make semen. The penis ejaculates semen during sexual activity.
Testicular cancer is a growth of cells that starts in the testicles. The testicles, which are also called testes, are in the scrotum. The scrotum is a loose bag of skin underneath the penis. The testicles make sperm and the hormone testosterone.
Testicular cancer isn't a common type of cancer. It can happen at any age, but it happens most often between the ages of 15 and 45.
The first sign of testicular cancer often is a bump or lump on a testicle. The cancer cells can grow quickly. They often spread outside the testicle to other parts of the body.
Testicular cancer is highly treatable, even when it spreads to other parts of the body. Treatments depend on the type of testicular cancer that you have and how far it has spread. Common treatments include surgery and chemotherapy.
Products & Services
Symptoms
Testicular lumps
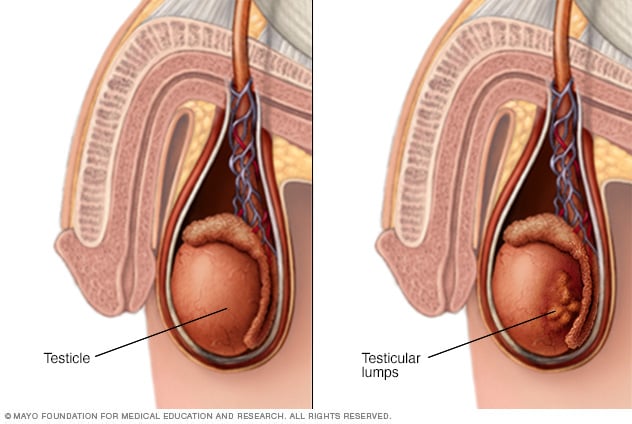
Testicular lumps
Pain, swelling or lumps in your testicle or groin area may be a sign or symptom of testicular cancer or other medical conditions requiring treatment.
Signs and symptoms of testicular cancer include:
- A lump or swelling in either testicle
- A feeling of heaviness in the scrotum
- A dull ache in the lower belly or groin
- Sudden swelling in the scrotum
- Pain or discomfort in a testicle or the scrotum
- Enlargement or tenderness of the breast tissue
- Back pain
Usually testicular cancer only happens in one testicle.
When to see a doctor
See your health care provider if you detect any symptoms that last longer than two weeks. These include pain, swelling or lumps in your testicles or groin area.
Causes
It's not clear what causes most testicular cancers.
Testicular cancer starts when something causes changes to the DNA of testicle cells. A cell's DNA holds the instructions that tell the cell what to do. The changes tell the cells to grow and multiply quickly. The cancer cells go on living when healthy cells would die as part of their natural life cycle. This causes a lot of extra cells in the testicle that can form a mass called a tumor.
In time, the tumor can grow beyond the testicle. Some cells might break away and spread to other parts of the body. Testicular cancer most often spreads to the lymph nodes, liver and lungs. When testicular cancer spreads, it's called metastatic testicular cancer.
Nearly all testicular cancers begin in the germ cells. The germ cells in the testicle make sperm. It's not clear what causes DNA changes in the germ cells.
Risk factors
Factors that may increase your risk of testicular cancer include:
- Having an undescended testicle, which is called cryptorchidism. The testes form in the belly during fetal development. They typically descend into the scrotum before birth. If you have a testicle that never descended, your risk of testicular cancer is higher. The risk is increased even if you've had surgery to move the testicle to the scrotum.
- Having a family history of testicular cancer. If testicular cancer runs in your family, you might have an increased risk.
- Being a young adult. Testicular cancer can happen at any age. But it's most common in teens and young adults between 15 and 45.
- Being white. Testicular cancer is most common in white people.
Prevention
There's no way to prevent testicular cancer. If you get testicular cancer, there's nothing you could have done to prevent it.
Testicular cancer screening
Some health care providers recommend regular testicle self-exams. During a testicular self-exam you feel your testicles for any lumps or other changes.
Not all health care providers agree with this recommendation. There's no research to show that self-exams can lower the risk of dying of testicular cancer. Even when it is found at a late stage, testicular cancer is likely to be cured.
Still, you might find it helpful to become aware of the usual feel of your testicles. You can do this by doing a testicular self-exam. If you notice any changes that last longer than two weeks, make an appointment with your health care provider.
Oct. 10, 2024