Diagnosis
EEG brain activity
EEG brain activity
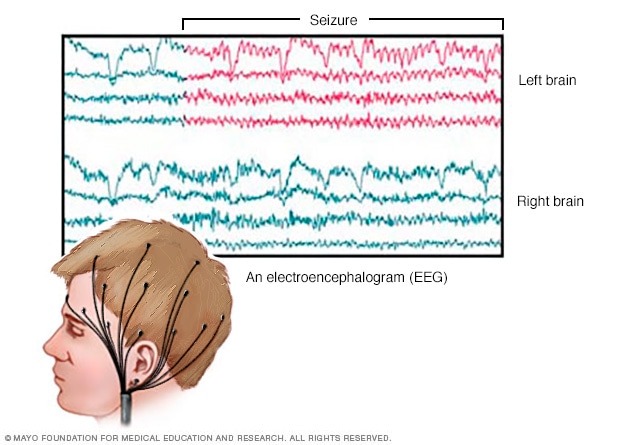
An EEG records the electrical activity of the brain through electrodes put on the scalp. EEG results show changes in brain activity. This may help diagnose brain conditions such as epilepsy and other seizure conditions.
High-density EEG

High-density EEG
During a high-density EEG test, a healthcare professional puts electrodes close together on the scalp. Like regular EEG, high-density EEG records brain activity. A high-density EEG test can help find the area in the brain where seizures happen.
CT scanner
CT scanner
A CT scan can show nearly all parts of the body. Healthcare professionals use it to diagnose disease or injury and to plan medical, surgical or radiation treatment.
Pinpointing seizure location
Pinpointing seizure location
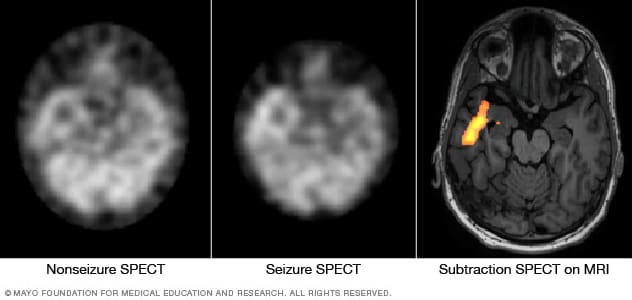
These SPECT images show the blood flow in the brain when there's no seizure activity (left) and during a seizure (middle). The subtraction SPECT coregistered to MRI (right) helps pinpoint the area of seizure activity by overlapping the SPECT results with brain MRI results.
After a seizure, your healthcare professional reviews your symptoms and medical history. You may have tests to find the cause of your seizure. Knowing the cause helps show how likely it is that you'll have another seizure.
Tests may include:
- Neurological exam. Your healthcare professional may test your behavior, motor abilities and mental function. This can show how well your brain and nervous system are working.
- Blood tests. A blood sample goes to a lab to check for signs of infection, genetic conditions, blood sugar levels and electrolyte imbalances.
- Electroencephalogram, also called EEG. Flat metal discs called electrodes attached to your scalp record the electrical activity of your brain. This shows up as wavy lines on an EEG recording. The EEG may show a pattern that tells whether a seizure is likely to happen again. An EEG also can help rule out other conditions that look like epilepsy.
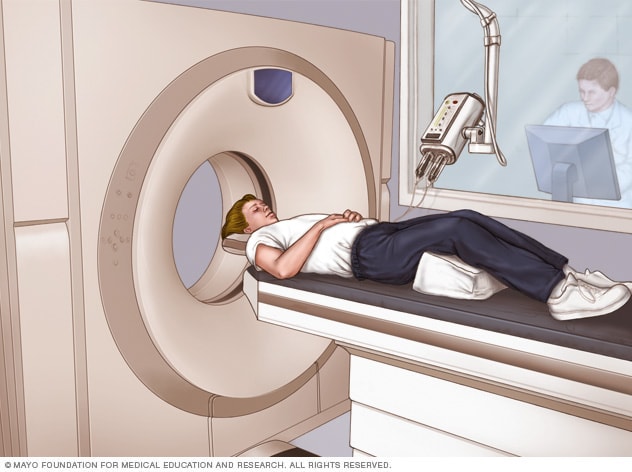
- Computerized tomography, also called CT. A CT scan uses X-rays to get cross-sectional images of the brain. CT scans can show what may be causing seizures. The scans can show tumors, bleeding and cysts.
- MRI. An MRI uses powerful magnets and radio waves to show a detailed view of the brain. An MRI can show possible causes of seizures.
- Positron emission tomography, also called PET. PET scans use a small amount of low-dose radioactive material. A healthcare professional puts the material into a vein. The scan shows active areas of the brain. PET scans can show where in the brain the seizure began.
- Single-photon emission computerized tomography, also called SPECT. A SPECT test uses a small amount of low-dose radioactive tracer. A healthcare professional puts the tracer into a vein. This makes a detailed, 3D map of the blood flow in the brain during a seizure. A form of a SPECT test called subtraction ictal SPECT coregistered with magnetic resonance imaging, also called SISCOM, may give even more-detailed results.
More Information
Treatment
Not everyone who has a seizure has another one. Your healthcare professional may decide not to start treatment until you've had more than one.
Seizure treatment aims to find the best therapy to stop your seizures with the fewest side effects.
Medications
Many medicines treat temporal lobe seizures. But many people can't manage seizures fully with medicines alone. Side effects are common. They can include tiredness, weight gain and dizziness.
Discuss possible side effects with your healthcare professional when thinking about treatments. Also ask what effect your seizure medicines may have on other medicines you take. For instance, some antiseizure medicines can affect how well birth control pills work.
Dietary therapy
Following a ketogenic diet can improve seizure management. A ketogenic diet is high in fat and very low in carbohydrates. But it can be hard to follow because it allows only a very limited number of foods.
Other versions of a high-fat, low-carbohydrate diet also may be helpful but not work as well. These diets include low glycemic index and Atkins diets. Experts are still studying these diets.
Surgical or other procedures
Implanted vagus nerve stimulation

Implanted vagus nerve stimulation
In vagus nerve stimulation, a device placed under the skin of the chest stimulates the vagus nerve in the neck. This sends signals to the brain that lessen seizures.
Deep brain stimulation
Deep brain stimulation
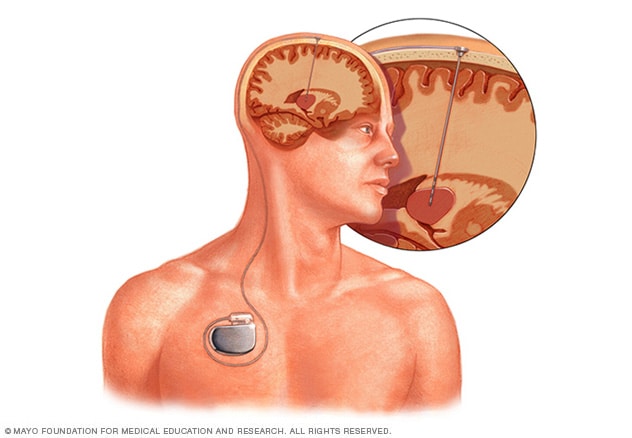
Deep brain stimulation involves putting an electrode deep within the brain. The amount of stimulation delivered by the electrode is controlled by a device placed under the skin in the chest. A wire that travels under the skin connects the device to the electrode.
When antiseizure medicines don't work, there are other treatments, including:
-
Surgery. Epilepsy surgery is a procedure to reduce seizures and improve the quality of life of people who have epilepsy. Surgeons often do this with open surgery to remove the area of the brain where seizures begin.
Sometimes, surgeons may be able to use MRI-guided laser therapy. This is a less- invasive way to destroy the area of tissue that causes seizures.
Surgery works best if you have seizures that always start in the same place in the brain. Most often, you won't have surgery if your seizures come from more than one area of the brain.
You also might not be able to have surgery if your healthcare team can't find where the seizures start. Surgery also may not be an option if your seizures come from a part of the brain that affects speech, thinking, movement, memories and other important functions.
- Vagus nerve stimulation. A device placed under the skin of the chest stimulates the vagus nerve in the neck. This sends signals to the brain that lessen seizures.
- Responsive neurostimulation. Surgeons place a device on the brain or in brain tissue. The device can tell when seizure activity starts. It sends electrical stimulation to stop the seizure.
- Deep brain stimulation. Surgeons place thin wires called electrodes in certain areas of the brain to produce electrical impulses. The impulses help the body manage the brain activity that causes seizures. The electrodes attach to a pacemakerlike device placed under the skin of the chest. The device manages how much stimulation happens.
Pregnancy and seizures
People who've had seizures can most often have healthy pregnancies. But some medicines used to treat seizures sometimes can cause health conditions that are present at birth.
Valproic acid is a medicine for generalized seizures that has been linked with cognitive issues and neural tube defects, such as spina bifida, in babies. The American Academy of Neurology recommends against using valproic acid during pregnancy because of risks to babies.
Talk with your healthcare professional about the risks of antiseizure medicines, including the risk of health conditions present at birth. Make a plan with your health professional before you get pregnant. Pregnancy can change the way you need to take your medicine.
Some people may need to change the dosage of seizure medicine before or during pregnancy. The goal is to be on the lowest dose of the safest seizure medicine that manages seizures.
Birth control and antiseizure medicines
Some antiseizure medicines keep birth control from working as well. Check with your healthcare professional to see whether your medicine affects your birth control. You may need to try other forms of birth control.
You see, an epileptic seizure is an abnormal electrical disturbance of the brain. The device is implanted under the skin, and four electrodes are attached to the outer layers of your brain. The device monitors brain waves, and when it senses abnormal electrical activity it fires electrical stimulation and stops the seizures.
Lifestyle and home remedies
Here are some steps you can take to help manage seizures:
- Take medicine correctly. Don't change the dose without first talking with your healthcare professional. If you think that your medicine needs a change, always talk with your health professional.
- Get enough sleep. Lack of sleep can trigger seizures. Be sure to get enough rest every night.
- Wear a medical alert bracelet. This helps emergency responders know how to treat you if you have a seizure.
- Ask your healthcare professional about driving. People who have seizures must be seizure-free for a certain length of time before being able to drive. The amount of time varies by state.
Personal safety
Most often, seizures don't result in serious injury. But injury is possible if you have recurrent seizures. These steps can help you avoid injury during a seizure:
- Take care near water. Don't swim alone or ride in a boat without someone nearby.
- Wear a helmet. Wear a helmet during activities such as bike riding or playing sports.
- Take showers. Don't take baths unless someone is near you.
- Soften your home. Pad sharp corners, buy furniture with rounded edges and choose chairs that have arms to keep you from falling off. Think about having carpet with thick padding to protect you if you fall.
- Have a list of seizure first-aid tips. Put them in a place where people can see them. Include phone numbers that people might need if you have a seizure.
Seizure first aid
It's helpful to know what to do if you see someone having a seizure. If you're at risk of having seizures in the future, give this information to family, friends and co-workers. Then they'll know what to do if you have a seizure.
To help someone during a seizure:
- Carefully roll the person onto one side.
- Place something soft under the person's head.
- Loosen tight neckwear.
- Don't put your fingers or other objects in the person's mouth.
- Don't try to restrain the person.
- Clear away dangerous objects if the person is moving.
- Stay with the person until medical help arrives.
- Watch the person closely so that you can tell medical helpers what happened.
- Time the seizure.
- Stay calm.
Coping and support
Stress due to living with a seizure condition can affect your mental health. Talk with your healthcare professional about your feelings. Look for ways to find help.
At home
Your family can provide much-needed support. Tell them what you know about your seizures. Let them know they can ask you questions. Ask them about their worries.
At work
Talk with your supervisor about your seizures and how they affect you. Discuss what you need your supervisor or co-workers to do if you have a seizure at work. Talk with your co-workers about seizures. This will help them understand your condition and give you more support.
You're not alone
Reach out to family and friends. Ask your healthcare professional about local support groups or join an online support community. Don't be afraid to ask for help. Having a strong support system is vital to living with any medical condition.
Preparing for your appointment
Sometimes seizures need medical help right away. There isn’t always time to prepare for an appointment.
But you may see your main healthcare professional or be sent to a specialist. You might see a specialist trained in brain and nervous system conditions, called a neurologist. Or you might see a neurologist trained in epilepsy, known as an epileptologist.
Here's some information to help you get ready for your appointment.
What you can do
- Write down what you remember about the seizure. Include when and where it happened, symptoms you had, and how long it lasted, if you know. Ask anyone who saw the seizure to help you fill in the details.
- Be aware of any restrictions before your appointment. When you make the appointment, ask if there's anything you need to do ahead of time to be ready for medical tests or exams.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you take, including doses.
- Take a family member or friend to your appointment. Someone who's with you can help you remember all the information you get. And the person who goes with you may be able to answer questions about your seizure that you can't.
- Write down questions to ask your healthcare professional. Making a list of questions can help you make the most of your time during your visit.
For seizures, some basic questions to ask include:
- What do you think caused my seizure?
- What tests do I need?
- What treatment do you suggest?
- How likely is it that I might have another seizure?
- How can I make sure that I don't hurt myself if I have another seizure?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Are there brochures or other printed material that I can have? What websites do you suggest?
Be sure to ask all the questions you have.
What to expect from your doctor
A healthcare professional is likely to ask you questions, such as:
- Can you describe your seizure episode?
- Was anyone there to see what happened?
- What did you feel just before the seizure? What about right after the seizure?
- Have you had a seizure or other neurological condition in the past?
- Do you have any family members who have been diagnosed with a seizure condition or epilepsy?
- Have you recently traveled outside the country?
Jan. 24, 2025