Hilar cholangiocarcinoma
Cholangiocarcinoma

Cholangiocarcinoma
Cholangiocarcinoma, also called bile duct cancer, happens in the tubes that carry the digestive fluid bile from the liver to the small intestine. The tubes are called bile ducts. When bile duct cancer forms in the ducts within the liver it's called intrahepatic cholangiocarcinoma. Bile duct cancer that happens in the ducts just outside the liver is called hilar cholangiocarcinoma. Bile duct cancer that happens near the small intestine is called distal cholangiocarcinoma.
Hilar cholangiocarcinoma is a type of cancer that starts as a growth of cells in the bile ducts. Bile ducts are slender tubes that carry the digestive fluid bile from the liver to the small intestine.
Cholangiocarcinoma is the medical term for bile duct cancer. Hilar cholangiocarcinoma is bile duct cancer that happens in a specific part of the bile ducts. Hilar cholangiocarcinoma happens where the bile ducts that lead out of the liver join with the duct that leads out of the gallbladder. These cancers also are known as perihilar cholangiocarcinomas or Klatskin tumors.
Hilar cholangiocarcinoma is the most common type of bile duct cancer, but it is still a rare form of cancer. Common symptoms include yellowing of the skin and the whites of the eyes, weight loss, stomach pain, and itching.
Treatment for hilar cholangiocarcinoma may include surgery to remove the cancer or a liver transplant. Other treatments may include chemotherapy, radiation therapy, immunotherapy and targeted therapy.
Symptoms
Hilar cholangiocarcinoma may not cause symptoms at first. Symptoms typically appear when the cancer grows and blocks the bile ducts. Signs and symptoms of hilar cholangiocarcinoma may include:
- Yellowing of the skin and the whites of the eyes, known as jaundice.
- Itching.
- Dark urine.
- Clay-colored stools.
- Stomach pain.
- Fatigue.
- Weight loss.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
Causes
Gallbladder and bile duct
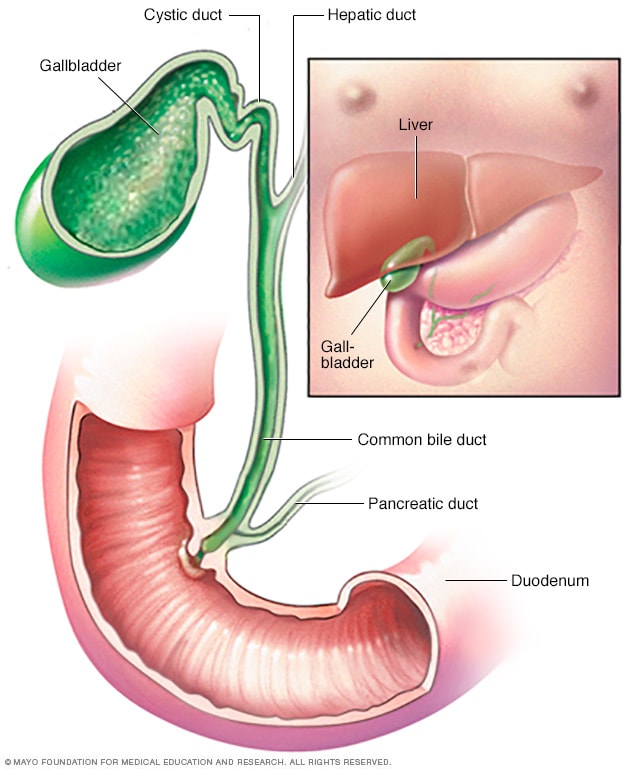
Gallbladder and bile duct
The gallbladder holds a yellow-green fluid called bile. Bile is made in the liver and flows into the gallbladder. It stays in the gallbladder until it's needed to help digest food. During eating, the gallbladder releases bile into the bile duct. The duct carries the bile to the upper part of the small intestine, called the duodenum, to help break down fat in food.
It's not clear what causes most hilar cholangiocarcinomas. This cancer starts in the bile ducts that connect the liver to the small intestine.
Hilar cholangiocarcinoma happens when cells in a bile duct develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to grow and multiply quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Risk factors
Factors that may increase the risk of hilar cholangiocarcinoma include:
- Primary sclerosing cholangitis. Primary sclerosing cholangitis causes hardening and scarring of the bile ducts that can lead to cancer.
- Older age. Hilar cholangiocarcinoma happens most often in adults over age 50.
- Inflammatory bowel disease. People who have ongoing inflammation of the digestive tract have an increased risk of hilar cholangiocarcinoma.
- Liver cirrhosis. Liver cirrhosis causes scarring of the liver that increases the risk of hilar cholangiocarcinoma.
- Bile duct cysts. Bile duct cysts cause dilated and irregular bile ducts. Having bile duct cysts increases risk of hilar cholangiocarcinoma.
- Gallbladder conditions. Ongoing inflammation of the gallbladder, called cholecystitis, increases the risk of hilar cholangiocarcinoma. People who develop gallstones also are at an increased risk.
- Liver parasites. In areas of Southeast Asia, hilar cholangiocarcinoma is linked to liver flukes, which are parasites that can infect humans. Liver fluke infection can happen from eating raw or undercooked fish.
Diagnosis
Hilar cholangiocarcinoma diagnosis often begins with a physical exam and a discussion of your health history. Imaging tests and blood tests may be used. A sample of tissue may be taken for lab testing.
Imaging tests
Imaging tests make pictures of the body. They can show the location and size of a hilar cholangiocarcinoma. Tests might include ultrasound, CT or MRI. Magnetic resonance cholangiopancreatography, also called MRCP, is often combined with other tests. It uses MRI to make detailed pictures of the liver, gallbladder, bile ducts and pancreas.
Liver function tests
Blood tests to measure your liver function can give your healthcare team clues about what's causing your symptoms.
Tumor marker tests
A tumor marker test looks for substances called tumor markers. These markers are often made by cancer cells or healthy cells in response to cancer. Checking the level of the tumor markers in your blood may give your healthcare team additional clues about your diagnosis.
Tumor markers for hilar cholangiocarcinoma include carbohydrate antigen 19-9, also called CA 19-9, and carcinoembryonic antigen, also called CEA. These are proteins that are overproduced by cholangiocarcinoma cells. Highly elevated numbers of these tumor markers may mean a more advanced cancer.
Having high levels of CA 19-9 and CEA in your blood doesn't always mean you have hilar cholangiocarcinoma. This also can happen with other bile duct conditions, such as bile duct inflammation and obstruction.
Biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. To get a sample of tissue from a hilar cholangiocarcinoma, a healthcare professional might use a procedure called endoscopic retrograde cholangiopancreatography, also called ERCP. During this procedure, a health professional puts a thin tube with a camera down the throat. The tube, called an endoscope, goes through the stomach and into the small intestine to get to the bile duct. The endoscope is used to put a dye into the bile duct to help show the bile ducts on X-rays. The X-ray images help guide the endoscope to the right place. A brush tool can extend from the endoscope to collect cells from the cancer.
Hilar cholangiocarcinoma staging
If you're diagnosed with hilar cholangiocarcinoma, the next step is to determine the cancer's extent, called the stage. Staging tests for hilar cholangiocarcinoma may include additional imaging tests, such as X-ray, MRI, CT and positron emission tomography, which also is called a PET scan. Your healthcare team uses the cancer staging test results to help create your treatment plan.
The stages of hilar cholangiocarcinoma range from 1 to 4. A stage 1 hilar cholangiocarcinoma is small and confined to the bile duct. As the cancer gets larger or spreads beyond the area it started in, the stages get higher. A stage 4 hilar cholangiocarcinoma has spread to many nearby lymph nodes or to other parts of the body.
Treatment
Treatment for hilar cholangiocarcinoma depends on the location and the extent of the cancer. Surgery may be used to remove the cancer. For some people, a liver transplant may be an option. Other treatments may include radiation therapy, radiofrequency ablation treatments and medicines. Medicines used to treat hilar cholangiocarcinoma include chemotherapy, targeted therapy and immunotherapy.
Your healthcare team considers many factors when creating a treatment plan. These factors may include your overall health, the type and stage of your cancer, and your preferences.
Surgery
The goal of surgery for hilar cholangiocarcinoma is to remove all of the cancer. Surgery may not be an option for everyone. This cancer grows near many important structures, which can make surgery difficult. When surgery is possible, options may include:
- Surgery to remove the cancer. Removing the cancer often includes removing and reconstructing part of the bile duct and nearby structures, such as the surrounding ducts and parts of the liver and gallbladder.
- Removing nearby lymph nodes. Lymph nodes may be removed to be tested for cancer. Removing cancerous lymph nodes may help prevent the spread of the cancer.
- Liver transplant. Sometimes surgery to remove the cancer is combined with a liver transplant. A surgeon removes the cancer and all of the liver. Then the surgeon puts a healthy liver from a donor into the body.
- Biliary drainage. Biliary drainage uses a procedure to restore the flow of bile if a bile duct is blocked by cancer. It might involve placing a thin tube into the bile duct to drain the bile. Sometimes a surgeon does a bypass surgery to reroute the bile duct around the cancer. Another kind of procedure might involve placing stents to hold open a bile duct being collapsed by cancer. Biliary drainage helps relieve symptoms of hilar cholangiocarcinoma.
Radiofrequency ablation
Radiofrequency ablation uses electric current to heat and destroy cancer cells. Using an imaging test such as ultrasound as a guide, a healthcare professional inserts one or more thin needles into small incisions in the belly. When the needles reach the cancer, they're heated with an electric current, destroying the cancer cells.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body.
For hilar cholangiocarcinoma, radiation therapy is sometimes combined with chemotherapy to kill cancer cells that remain after surgery. Radiation therapy also may be combined with chemotherapy to treat cancer that has spread to the lymph nodes.
Sometimes the healthcare team uses other procedures to place the radiation close to the cancer. One way to do this is with radioembolization. It involves putting small beads that hold radiation into a blood vessel that leads to the cancer. The beads travel through the blood vessel and block the blood supply to the cancer. The beads give off radiation directly to the cancer.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Most chemotherapy medicines are given through a vein. Some come in pill form.
For hilar cholangiocarcinoma, chemotherapy may be used after surgery to kill any remaining cancer cells. For those with advanced cancer that can't be removed with surgery, chemotherapy may be an option to slow the growth of the cancer.
Chemotherapy is sometimes combined with radiation therapy after surgery to kill any remaining cancer cells. Chemotherapy also may be combined with radiation to treat cancer that has spread to the lymph nodes.
Targeted therapy
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. For those with advanced hilar cholangiocarcinoma that can't be removed with surgery, targeted therapy may be an option. Some cancer cells might be tested to see if targeted therapy is likely to work on the cancer.
Immunotherapy
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells, such as cancer cells, that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells. For those with advanced hilar cholangiocarcinoma that can't be removed with surgery, immunotherapy may be an option.
Palliative care
Palliative care is a special type of healthcare that helps you feel better when you have a serious illness. If you have cancer, palliative care can help relieve pain and other symptoms. A healthcare team that may include doctors, nurses and other specially trained health professionals provides palliative care. The care team's goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time you're getting strong cancer treatments, such as surgery, chemotherapy, immunotherapy, targeted therapy or radiation therapy.
The use of palliative care with other treatments can help people with cancer feel better and live longer.
Coping and support
With time, you'll find ways to cope with feelings that happen after a cancer diagnosis. Until then, here are some ideas for coping with hilar cholangiocarcinoma.
Learn enough about cancer to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you want, your prognosis. As you learn more about hilar cholangiocarcinoma, you may become more confident in making treatment decisions.
Keep friends and family close
Keeping your close relationships strong can help you deal with hilar cholangiocarcinoma. Friends and family can provide the practical support you may need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and worries. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the U.S. National Cancer Institute and the American Cancer Society.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks you might have hilar cholangiocarcinoma, you may be referred to a doctor who specializes in diseases of the digestive system, called a gastroenterologist. If a cancer diagnosis is made, you also may be referred to a doctor who specializes in treating cancer, called an oncologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For hilar cholangiocarcinoma, some basic questions to ask include:
- Do I have hilar cholangiocarcinoma?
- What is the stage of my hilar cholangiocarcinoma?
- Has my hilar cholangiocarcinoma spread to other parts of my body?
- Will I need more tests?
- What are the treatment options?
- How much does each treatment increase my chances of a cure or prolong my life?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- Is there one treatment option you believe is the best?
- What would you recommend to a friend or family member in my situation?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?