Diagnosis
If you have unusual urges to urinate, your healthcare professional checks for an infection or blood in your urine. Your health professional also may check to see if you're emptying your bladder all the way when you urinate.
Your appointment will likely include a:
- Medical history.
- Neurological exam to look for sensory issues or reflex problems.
- Physical exam, which may include a rectal exam and a pelvic exam in women.
- Urine sample to test for infection, traces of blood or other issues.
Tests of bladder function
Your health professional may suggest tests to see how well your bladder works and whether it can empty all the way, called urodynamic tests. A specialist most often does these tests. But testing may not be needed to make a diagnosis or begin treatment.
Urodynamic tests include:
-
Measuring urine left in the bladder. This test is important if you might not be emptying your bladder all the way when you urinate. Remaining urine in the bladder, called postvoid residual urine, can cause symptoms like those of an overactive bladder.
To measure residual urine after you void, your health professional may want an ultrasound scan of your bladder. The ultrasound scan translates sound waves into an image. The image shows how much urine is left in your bladder after you urinate.
Sometimes, a thin tube, called a catheter, is passed through the urethra and into your bladder to drain the remaining urine. Then the urine can be measured.
- Measuring urine flow rate. To measure how much and how fast you urinate, you may be asked to urinate into a device called a uroflowmeter. A uroflowmeter catches and measures the urine. It then uses the data to create a graph of changes in your flow rate.
Testing bladder pressures. A test called cystometry measures pressure in your bladder and in the area around it as your bladder fills. After emptying your bladder with a thin tube called a catheter, your health professional uses another catheter to fill your bladder slowly with warm fluid.
Another catheter with a sensor that measures pressure goes into the rectum or the vagina. The sensor tells how much pressure your bladder uses to empty all the way.
This procedure can show how full your bladder is when you start needing to urinate. It also can show whether your bladder tightens when it's not supposed to.
Your health provider reviews the results of your tests with you and suggests a treatment plan.
Treatment
A mix of treatments may be best to relieve overactive bladder symptoms.
Behavioral therapies
Female pelvic floor muscles
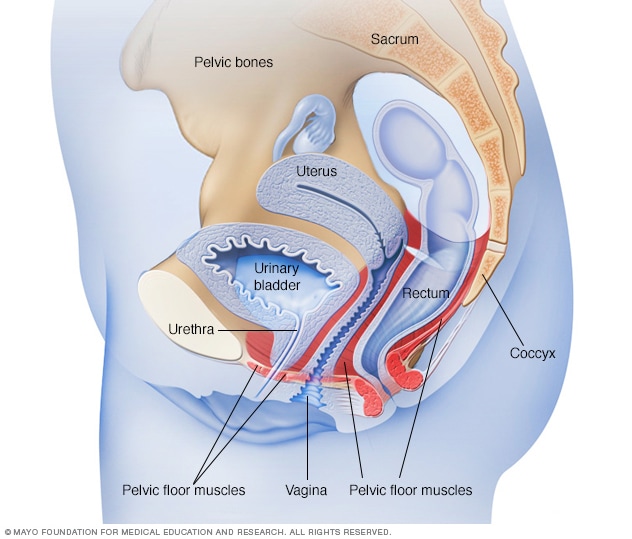
Female pelvic floor muscles
The pelvic floor muscles support the pelvic organs. Those organs include the uterus, bladder and rectum. Kegel exercises can help strengthen the pelvic floor muscles.
Male pelvic floor muscles
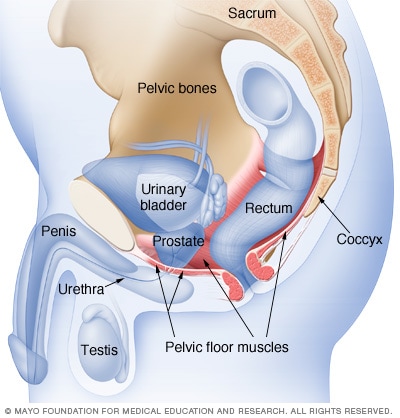
Male pelvic floor muscles
The male pelvic floor muscles support the bladder and bowel and affect sexual function. Kegel exercises can help strengthen these muscles.
Behavioral therapies are the first choice in helping manage an overactive bladder. They often work and have no side effects. Behavioral therapies may include:
- Biofeedback. During biofeedback, an electrical patch put on the skin over your bladder is attached to a wire that's linked to a screen. This lets you see when your bladder muscles contract. This can help you know what it feels like when the muscles tighten so you can learn to control them.
- Bladder training. Bladder training involves going to the bathroom at set times. Use a bladder diary to see how often you go. Then add 15 minutes at a time between trips to the toilet. Urinate even if you don't feel the urge. This can train your bladder to hold more urine before you feel the urge to urinate.
- Healthy weight. If you're overweight, losing weight may ease symptoms. Weight loss may help if you also have stress urinary incontinence.
- Intermittent catheterization. If you are not able to empty your bladder well, using a tube called a catheter at times to empty your bladder all the way helps your bladder do what it can't do by itself. Ask your healthcare professional if this approach is right for you.
-
Pelvic floor muscle exercises. Kegel exercises strengthen your pelvic floor muscles and urinary sphincter. Stronger muscles can help you stop the bladder from contracting on its own.
Your healthcare professional or a physical therapist can help you learn to do Kegel exercises. Kegel exercises are like other types of exercise. How well they work depends on your doing them regularly. It can take six weeks before they start to work.
Medications
After menopause, vaginal estrogen therapy can help strengthen the muscles and tissues in the urethra and vaginal area. Vaginal estrogen comes in creams, suppositories, tablets or rings. It can improve symptoms of overactive bladder.
Medicines that relax the bladder can help relieve symptoms of overactive bladder and reduce episodes of urge incontinence. These drugs include:
- Fesoterodine (Toviaz).
- Mirabegron (Myrbetriq).
- Oxybutynin, which can be taken as a pill (Ditropan XL) or used as a skin patch (Oxytrol) or gel (Gelnique).
- Solifenacin (Vesicare).
- Tolterodine (Detrol).
- Trospium.
- Vibegron (Gemtesa).
Common side effects of most of these drugs include dry eyes and dry mouth. But drinking water for thirst can make symptoms of overactive bladder worse. Constipation is another possible side effect that can make bladder symptoms worse. Extended-release forms of these medicines, including the skin patch or gel, may cause fewer side effects.
Your healthcare professional may suggest that you sip small amounts of water or suck on a piece of sugar-free candy or chew sugar-free gum to relieve dry mouth. You might use eyedrops to keep your eyes moist.
Medicines available without a prescription, such mouthwashes designed to relieve dry mouth, can be helpful for long-term dry mouth. Eating a fiber-rich diet or using stool softeners might help prevent constipation.
Bladder injections
OnabotulinumtoxinA (ON-ah-boch-yoo-lih-num-tox-in-A), also called Botox, is a protein from the bacteria that cause botulism illness. Small doses shot into bladder tissues can relax the muscles and increase the amount of urine the bladder can hold.
Studies show that Botox may help severe urge incontinence. The effects most often last six months or more. When the effects wear off, you need another shot.
Side effects from these shots include urinary tract infections and retaining urine. If you're thinking of Botox treatments, you must be willing to put a catheter in yourself if you start retaining urine.
Nerve stimulation
Sacral nerve stimulator
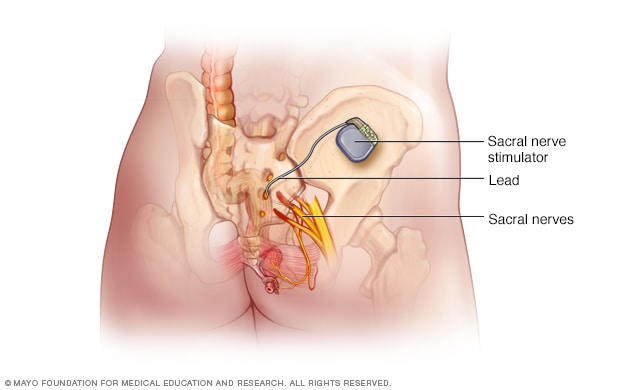
Sacral nerve stimulator
During sacral nerve stimulation, a surgically implanted device delivers electrical impulses to the nerves that regulate bladder activity. These are called the sacral nerves. The unit is placed under the skin in the lower back, about where the back pocket is on a pair of pants. In this image, the device is shown out of place to allow a better view of the unit.
Mild electrical pulses to the bladder nerves can improve overactive bladder symptoms.
One procedure uses a thin wire placed near the sacral nerves where they pass near your tailbone. The sacral nerves carry signals to your bladder.
This minimally invasive procedure is often done with a trial of a wire put under the skin in your lower back. Your healthcare professional then uses a hand-held device attached to the wire to send electrical impulses to your bladder. This is like what a pacemaker does for the heart.
If the trial helps your symptoms, a battery-powered pulse generator is put in with surgery. The device stays in your body to help control the nerves.
Percutaneous tibial nerve stimulation (PTNS)
This procedure uses a thin needle that is put through the skin near the ankle. It sends electrical stimulation from a nerve in the leg, called the tibial nerve, to the spine. There it connects with the nerves that control the bladder.
PTNS treatments are given once a week for 12 weeks to treat symptoms of overactive bladder. After that, treatments every 3 to 4 weeks help keep symptoms under control.
Surgery
Surgery to treat overactive bladder is only for people with severe symptoms who don't respond to other treatments. The goal is to improve the bladder's ability to store urine and reduce pressure in the bladder.
Procedures include:
- Surgery to increase how much the bladder can hold. This procedure uses pieces of the bowel to replace a part of the bladder. People who have this surgery may need to use a catheter sometimes for the rest of their lives to empty their bladder.
- Bladder removal. This procedure is used as a last resort. It involves removing the bladder and surgically making a bladder to replace it, called a neobladder. Or it might involve making an opening in the body, called a stoma, to attach a bag on the skin to collect urine.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
The following might reduce overactive bladder symptoms:
- Not drinking too much or too little. Ask your healthcare professional how much to drink daily. Drinking too much fluid can make your symptoms worse. But not drinking enough can bother the lining of your bladder and increase the urge to urinate.
- Limit foods and drinks that might bother your bladder. These include caffeine, alcohol, tea, carbonated drinks, citrus juice and fruit, chocolate, spicy foods, and tomatoes. Try not eating or drinking these to see if it helps.
- Maintain a healthy weight. If you're overweight, losing weight may ease your symptoms. Heavier people also are at greater risk of stress urinary incontinence. That also may improve with weight loss.
- Manage constipation. Constipation can make urinary incontinence worse. Your healthcare professional might suggest that you add more fiber to your diet. You can add fiber by eating more high-fiber foods or by taking a fiber supplement.
- Quit smoking. Smoking can make urinary incontinence worse. If you smoke, ask your healthcare professional for help with quitting.
- Wear absorbent pads or underwear. These are designed to take in liquids, control odor and protect your clothing when urine leaks.
Alternative medicine
No complementary or alternative therapies have been proved to treat overactive bladder.
Some research suggests that acupuncture might help ease the symptoms of overactive bladder. Acupuncture involves using very thin needles that are thrown out after the procedure. More study is needed.
Complementary treatments may not be covered by insurance. So check with your insurance company if you want to try one.
Coping and support
Living with overactive bladder can be hard. Consumer education and advocacy support groups such as the National Association for Continence can provide you with online resources and information. These groups connect you with other people who have overactive bladder and urge incontinence. Support groups offer the chance to talk about your worries and learn new ways to cope.
Teaching your family and friends about overactive bladder and how it affects you may help you create your own support network and reduce feelings of shame. Once you start talking about it, you may be surprised to learn how common this condition really is.
Preparing for your appointment
For overactive bladder, start by seeing your primary healthcare professional. You might then be sent to a specialist in urinary conditions in men and women, called a urologist, a specialist in urinary conditions in women, called a urogynecologist, or a specialist in physical therapy.
Here's some information to help you get ready for your appointment.
What you can do
- Keep a bladder diary for a few days. Write down when, how much and what kind of fluids you drink; when you urinate; whether you feel an urge to urinate; and whether you have incontinence.
- Tell your healthcare professional how long you've had your symptoms and how they affect your day-to-day activities.
- Note other symptoms you have, especially those related to how your bowels work.
- Let your health professional know if you have diabetes or a neurological disease, or if you've had pelvic surgery or radiation treatments.
- Make a list of all the medicines, vitamins or supplements you take, including doses.
- Write down questions to ask your healthcare professional.
For overactive bladder, questions might include:
- What are the possible causes of my symptoms?
- Is my urine clear?
- Do I empty my bladder well?
- Do you recommend other tests? For what?
- What treatments are there? Which do you suggest for me?
- What side effects can I expect from treatment?
- Are there any dietary changes that could help?
- How do my other health problems affect my bladder symptoms?
- Are there brochures or other printed material I can have? What websites do you suggest?
What to expect from your doctor
Your healthcare professional may use an overactive bladder questionnaire to assess your symptoms. Questions might include:
- How long have you had these symptoms?
- Do you leak urine? How often?
- What do your symptoms keep you from doing?
- Does movement such as walking, coughing or bending over cause you to leak urine?
Feb. 04, 2025