Diagnosis
To find out if you have low blood pressure, also called hypotension, your healthcare professional gives you a physical exam. You're also asked questions about your medical history. The exam includes checking your blood pressure.
You also can measure your blood pressure at home. Checking your blood pressure at home can help your healthcare professional diagnose high blood pressure earlier than usual. Ask a member of your healthcare team to:
- Help you pick a blood pressure monitor.
- Tell you how often to check your blood pressure.
- Explain what blood pressure numbers should prompt you to call the medical office right away.
If you get a home blood pressure reading at or just below 90/60 mm Hg, it's not always a cause for concern. Your healthcare professional might tell you that the reading is OK for you, especially if you have no symptoms.
Tests
Tilt table test
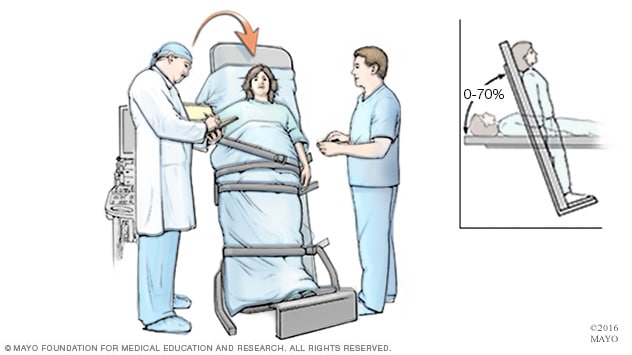
Tilt table test
Someone having a tilt table test begins by lying flat on a table. Straps hold the person in place. After lying flat for a while, the table is tilted to a position that mimics standing. The healthcare professional watches how the heart and the nervous system that controls it respond to the changes in position.
Other tests may be done to find out the cause of low blood pressure.
- Blood tests. Blood tests can help find symptoms of other conditions that can lower blood pressure. These include low blood sugar, also called hypoglycemia; high blood sugar, also called hyperglycemia or diabetes; and a low red blood cell count, also called anemia.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. During an ECG, sensors called electrodes are attached to the chest and sometimes to the arms or legs. Wires attached to the sensors connect to a machine that displays or prints out results. An ECG shows how fast or slow the heart is beating. It can be used to detect a current or previous heart attack.
- Tilt table test. A tilt table test can study how the body reacts to changes in position. The test involves lying on a table that's tilted to raise the upper part of the body. This mimics the movement from lying down to standing up. Straps hold the body in place. Heart rate and blood pressure are tracked during the test.
More Information
Treatment
Compression stockings
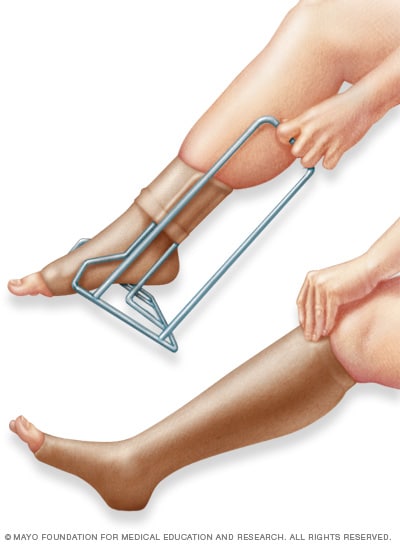
Compression stockings
Compression stockings, also called support stockings, press on the legs, improving blood flow. A stocking butler may help with putting on the stockings.
Low blood pressure without symptoms or with only mild symptoms rarely requires treatment.
If low blood pressure causes symptoms, the treatment depends on the cause. For instance, if medicine causes low blood pressure, your healthcare professional may recommend changing or stopping the medicine. Or the dose of medicine might be lowered. Don't change or stop taking your medicine without first talking to your healthcare professional.
If the cause of low blood pressure isn't clear or if no treatment exists, the goal is to raise blood pressure and relieve symptoms. Depending on your age, health and the type of low blood pressure you have, there are various ways to do this:
- Use more salt. Experts usually recommend limiting table salt and foods high in sodium. That's because salt and sodium can raise blood pressure, sometimes by a lot. For people with low blood pressure, though, that can be a good thing. But too much salt or sodium can lead to heart failure, especially in older adults. So it's important to check with a healthcare professional before eating more salt or high-sodium foods.
- Drink more water. Fluids increase blood volume and help prevent dehydration, both of which are important in treating hypotension.
- Wear compression stockings. Also called support stockings, these elastic stockings are often used to relieve the pain and swelling of varicose veins. They improve blood flow from the legs to the heart. Some people have an easier time using compression belts around the stomach area than they do using compression stockings. The compression belts are called abdominal binders.
Medicines. Various medicines can treat low blood pressure that occurs when standing up, also called orthostatic hypotension. For example, the drug fludrocortisone boosts blood volume. It's often used to treat orthostatic hypotension.
If you have long-term orthostatic hypotension, midodrine (Orvaten) may be prescribed to raise standing blood pressure levels. This medicine lessens the ability of the blood vessels to expand, which raises blood pressure.
Lifestyle and home remedies
Depending on the reason for low blood pressure, the following lifestyle and home remedies might help ease or prevent symptoms:
- Drink more water, less alcohol. Alcohol is dehydrating and can lower blood pressure, even in moderation. Water boosts the amount of blood in the body and prevents dehydration.
Pay attention to body positions. Gently move from lying flat or squatting to a standing position. Don't sit with legs crossed.
If symptoms of low blood pressure begin while standing, cross the thighs like a pair of scissors and squeeze. Or put one foot on a ledge or chair and lean as far forward as you can. These moves encourage blood flow from the legs to the heart.
Eat small, low-carb meals. To help prevent blood pressure from dropping sharply after meals, eat small meals several times a day. Limit high-carbohydrate foods such as potatoes, rice, pasta and bread.
A healthcare professional also might recommend drinking one or two strong cups of caffeinated coffee or tea with breakfast. Caffeine can cause dehydration, though, so be sure to drink plenty of water and other fluids without caffeine.
- Exercise regularly. As a general goal, work up to at least 150 minutes of moderate aerobic exercise a week. For example, you could aim to get about 30 minutes of activity most days. Also, aim to do strength-training exercises at least twice a week. But try not to exercise in hot, humid conditions.
Preparing for your appointment
You don't have to take any special steps to prepare to have your blood pressure checked. Don't stop taking medicines you think might affect your blood pressure without a healthcare professional's advice.
Here's some information to help you get ready for your appointment.
What you can do
Make a list of:
- Symptoms. Include any that do not seem related to low blood pressure, and when they occur.
- Blood pressure readings. If you track your blood pressure at home, keep a log of your blood pressure readings. Note multiple readings at different times of day. Also note when you have symptoms and whether they happened when your blood pressure was low.
- Important personal information. Include any family history of low blood pressure and major stresses or recent life changes.
- All medicines, vitamins or other supplements you use. Include the doses you take.
- Questions to ask your healthcare professional.
For low blood pressure, basic questions to ask your healthcare professional include:
- What is likely causing my symptoms or condition?
- What are other possible causes?
- What tests will I need?
- What's the most appropriate treatment?
- How often should I be screened for low blood pressure?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed materials I can have? What websites do you recommend?
Feel free to ask other questions.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, including:
- Do you always have symptoms of low blood pressure, or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to make your symptoms worse?
- Do you have a family history of heart disease?