Overview
Keratoconus
Keratoconus
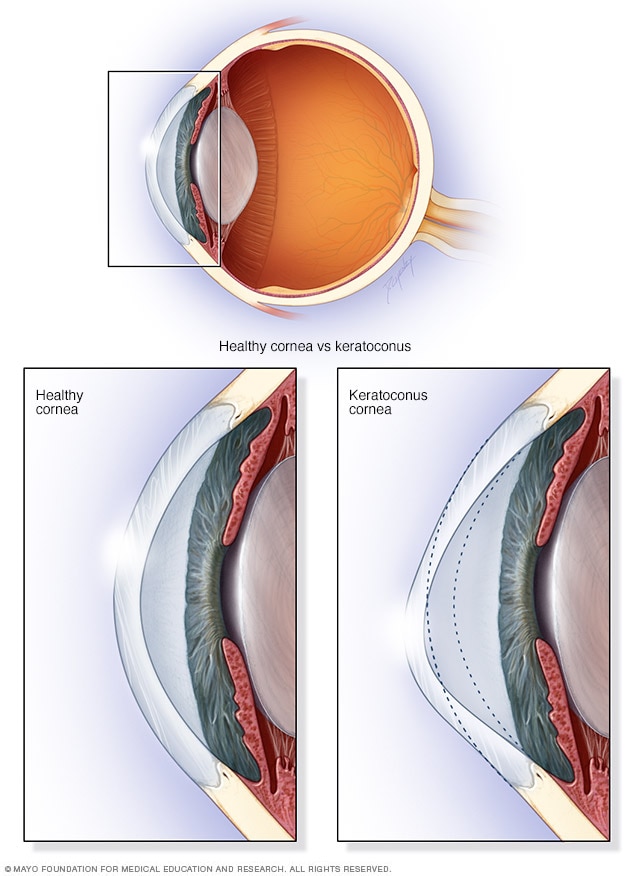
In keratoconus, your cornea thins and gradually bulges outward into a cone shape. This can cause blurry, distorted vision.
Keratoconus (ker-uh-toe-KOH-nus) is an eye condition in which the clear, dome-shaped front of the eye, called the cornea, gets thinner, steeper and bulges outward into a cone shape.
A cone-shaped cornea causes blurred vision and may cause sensitivity to light and glare. Keratoconus usually affects both eyes. However, it can affect one eye more than the other. It generally begins to affect people between the late teens and 30 years of age. The condition may progress slowly for 10 years or longer.
In the early stages of keratoconus, you might be able to correct vision problems with glasses or soft contact lenses. Later, you may have to be fitted with rigid, gas permeable contact lenses or other types of lenses, such as scleral lenses. If your condition gets worse, you may need a cornea transplant.
A procedure called corneal collagen cross-linking may help to slow or stop keratoconus from progressing, possibly preventing the need for a future cornea transplant. This treatment may be offered in addition to the vision correction options above.
Symptoms
Symptoms of keratoconus may change as the disease progresses. They include:
- Blurred or distorted vision.
- Increased sensitivity to bright light and glare, which can cause problems with night driving.
- A need for frequent changes in eyeglass prescriptions.
- Sudden worsening or clouding of vision.
When to see a doctor
See your eye doctor if your eyesight is worsening rapidly. This might be caused by an irregular curvature of the eye, called astigmatism. Your eye doctor also may look for signs of keratoconus during routine eye exams.
Causes
No one knows what causes keratoconus, although genetic and environmental factors are thought to be involved. Around 1 in 10 people with keratoconus also has a parent with the condition.
Risk factors
These factors can increase the risk of developing keratoconus:
- Having a family history of keratoconus.
- Rubbing the eyes vigorously.
- Having certain conditions, such as retinitis pigmentosa, Down syndrome, Ehlers-Danlos syndrome, Marfan syndrome, hay fever and asthma.
Complications
In some situations, the cornea may swell quickly and cause sudden reduced vision and scarring of the cornea. This is caused by a condition in which the inside lining of the cornea, called Descemet's membrane, breaks down. This causes fluid to enter the cornea, a condition known as hydrops. The swelling usually goes down by itself, but a scar may form that affects vision.
Advanced keratoconus also may cause the cornea to become scarred, particularly where the cone is most prominent. A scarred cornea causes worsening vision problems and may require cornea transplant surgery.