Diagnosis
A diagnosis of hydrocephalus is usually based on:
- Your symptoms.
- A general physical exam.
- A neurological exam.
- Brain-imaging tests.
Neurological exam
The type of neurological exam depends on a person's age. A health care professional might ask questions and conduct simple tests to judge muscle condition, movement, well-being and function of sensory abilities.
Brain imaging
Imaging tests can help diagnose hydrocephalus. They also can pinpoint underlying causes of symptoms. Imaging tests include:
- Ultrasound. This test is often the first test for infants because it's a simple, low-risk procedure. The ultrasound device is placed over the soft spot on the top of the baby's head. Ultrasound also might find hydrocephalus before birth during routine prenatal exams.
-
MRI. This test uses radio waves and a magnetic field to produce detailed images of the brain. This test is painless, but it is noisy and requires lying still.
MRI scans can show enlarged ventricles caused by excess cerebrospinal fluid. MRI also can be used to find causes of hydrocephalus or other conditions contributing to symptoms.
Children might need medicine to help them feel calm, known as mild sedation, for some MRI scans. However, some hospitals use a fast version of MRI that usually doesn't require sedation.
CT scan. This specialized X-ray technology produces cross-sectional views of the brain. Scanning is painless and quick. But this test also requires lying still, so a child usually receives a mild sedative.
CT scans show less detail than do MRI scans. And CT technology causes exposure to a small amount of radiation. CT scans for hydrocephalus usually are used only for emergency exams.
Treatment
One of two surgical treatments can be used to treat hydrocephalus.
Shunt
Shunt system
Shunt system
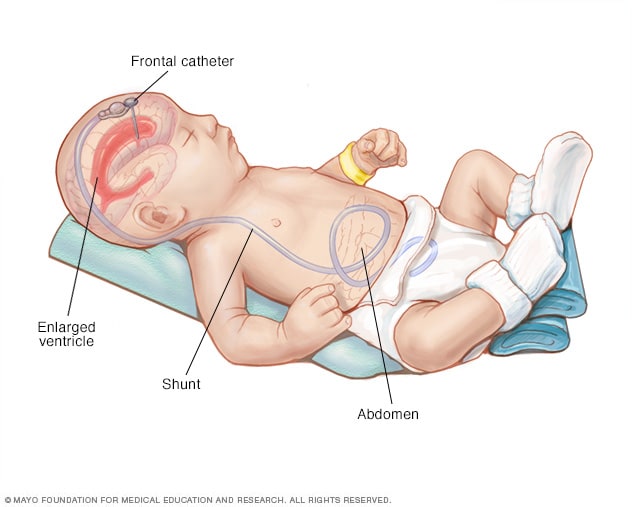
A shunt drains excess cerebrospinal fluid from the brain to another part of the body, such as the stomach, where it can be more easily absorbed.
The most common treatment for hydrocephalus is the surgical insertion of a drainage system, called a shunt. It consists of a long, flexible tube with a valve that keeps fluid from the brain flowing in the right direction and at the proper rate.
One end of the tubing is usually placed in one of the brain's ventricles. The tubing is then tunneled under the skin to another part of the body such as the stomach or a heart chamber. This allows excess fluid to be more easily absorbed.
People who have hydrocephalus usually need a shunt system for the rest of their lives. They require regular monitoring.
Endoscopic third ventriculostomy
Some people may have a surgery called endoscopic third ventriculostomy. The surgeon uses a small video camera to see inside the brain. Then the surgeon makes a hole in the bottom of a ventricle. This allows cerebrospinal fluid to flow out of the brain.
Complications of surgery
Both surgical procedures can result in complications. Shunt systems can stop draining cerebrospinal fluid. Or shunt systems may poorly regulate drainage because of mechanical problems, a blockage or infections. Complications of ventriculostomy include bleeding and infections.
Complications of surgery require prompt attention. Another surgery or other interventions may be needed. Fever or symptoms of hydrocephalus should prompt an appointment with your health care professional.
Other treatments
Some people with hydrocephalus, particularly children, might need supportive therapies. Need for these therapies depends on the long-term complications of hydrocephalus.
Children's care teams might include:
- Pediatrician or physiatrist, who oversees the treatment plan and medical care.
- Pediatric neurologist, who specializes in diagnosing and treating neurological conditions in children.
- Occupational therapist, who specializes in therapy to develop everyday skills.
- Developmental therapist, who specializes in therapy to help your child develop age-appropriate behaviors, social skills and interpersonal skills.
- Mental health professional, such as a psychologist or psychiatrist.
- Social worker, who helps the family get needed services and plan for transitions in care.
Children who are in school may need special education. Special education teachers address learning disabilities, determine educational needs and help find needed resources.
Adults with more serious complications might need the services of occupational therapists or social workers. Or they may need to see specialists in dementia care or other medical specialists.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
With the help of therapies and educational services, many people with hydrocephalus live with few limitations.
If you have a child with hydrocephalus, there are many resources available to provide emotional and medical support. Children with developmental disabilities might be eligible for government-sponsored health care and other support services. Check with your state or county social services agency.
Hospitals and organizations serving people with disabilities are good resources for emotional and practical support. Members of your health care team also can help. Ask for help connecting with other families who are coping with hydrocephalus.
Adults living with hydrocephalus might find valuable information from organizations dedicated to hydrocephalus education and support, such as the Hydrocephalus Association.
Should you be vaccinated against meningitis?
Ask your child's or your health care team if you or your child should receive a vaccine against meningitis, once a common cause of hydrocephalus. The Centers for Disease Control and Prevention recommends meningitis vaccination for preteen children and boosters for teenagers. Vaccination also is recommended for younger children and adults who might be at increased risk of meningitis for any of the following reasons:
- Traveling to countries where meningitis is common.
- Having an immune system disease called terminal complement deficiency.
- Having a damaged spleen or having had the spleen removed.
- Living in a college dormitory.
- Joining the military.
Preparing for your appointment
The timing of diagnosing a child with hydrocephalus can depend on how bad the symptoms are and when problems appeared. It also may depend on whether there were risk factors for hydrocephalus during the pregnancy or delivery. Sometimes hydrocephalus can be diagnosed at birth or before birth.
Well-baby visits
It's important to take your child to all regularly scheduled well-baby visits. Health care professionals monitor your child's development in key areas, including:
- Head size, rate of head growth and overall body growth.
- Muscle strength and tone.
- Coordination.
- Posture.
- Age-appropriate motor skills.
- Sensory abilities such as vision, hearing and touch.
Questions you should be prepared to answer during regular checkups might include:
- What concerns do you have about your child's growth or development?
- How well does your child eat?
- How does your child respond to touch?
- Is your child reaching certain milestones in development, such as rolling over, pushing up, sitting up, crawling, walking or speaking?
Preparing for other health care visits
You'll likely start by seeing your child's or your health care professional. You may then be referred to a doctor who specializes in brain and nervous system conditions, known as a neurologist.
Be prepared to answer the following questions about your symptoms or on your child's behalf:
- What symptoms have you noticed? When did they begin?
- Have these symptoms changed over time?
- Do these symptoms include nausea or vomiting?
- Have you or your child had any vision problems?
- Have you or your child had a headache or fever?
- Have you noticed personality changes, including increased irritability?
- Has your child's school performance changed?
- Have you noticed new problems with movement or coordination?
- Is your child having trouble sleeping or lacking in energy?
- Has your infant had seizures?
- Has your infant had problems with eating or breathing?
- In older children and adults, have symptoms included loss of bladder control and urinating often?
- Have you or your child had a recent head injury?
- Have you or your child recently begun a new medicine?
Sept. 15, 2023