Overview
Typical heartbeat
Typical heartbeat
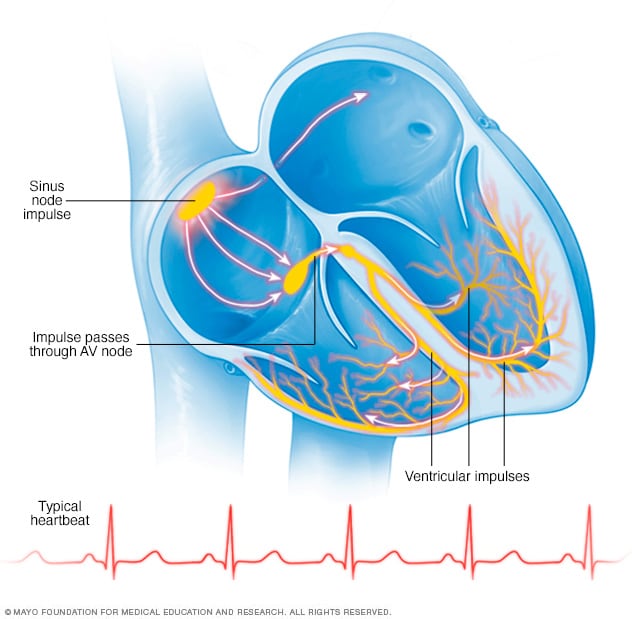
In a typical heart rhythm, a tiny cluster of cells at the sinus node sends out an electrical signal. The signal then travels through the atria to the atrioventricular (AV) node and then passes into the ventricles, causing them to contract and pump out blood.
A heart arrhythmia (uh-RITH-me-uh) is an irregular heartbeat. A heart arrhythmia occurs when the electrical signals that tell the heart to beat don't work properly. The heart may beat too fast or too slow. Or the pattern of the heartbeat may be inconsistent.
A heart arrhythmia may feel like a fluttering, pounding or racing heartbeat. Some heart arrhythmias are harmless. Others may cause life-threatening symptoms.
There are times when it is OK to have a fast or slow heartbeat. For example, the heart may beat faster with exercise or slow down during sleep.
Heart arrhythmia treatment may include medicines, devices such as pacemakers, or a procedure or surgery. The goals of treatment are to control or get rid of fast, slow or otherwise irregular heartbeats. A heart-healthy lifestyle can help prevent heart damage that can trigger some heart arrhythmias.
Types
In general, heart arrhythmias are grouped by the speed of the heart rate. For example:
- Tachycardia (tak-ih-KAHR-dee-uh) is a fast heartbeat. The heart rate is greater than 100 beats a minute.
- Bradycardia (brad-e-KAHR-dee-uh) is a slow heartbeat. The heart rate is less than 60 beats a minute.
Fast heartbeat, called tachycardia
Types of tachycardias include:
- Atrial fibrillation (AFib). Chaotic heart signaling causes a rapid, uncoordinated heartbeat. AFib may be temporary and start and stop on its own. But some episodes may not stop unless treated. AFib has been linked to stroke.
- Atrial flutter. Atrial flutter is similar to AFib, but the heartbeats are more organized. Atrial flutter also is linked to stroke.
- Supraventricular tachycardia. This broad term includes irregular heartbeats that start above the lower heart chambers, called the ventricles. Supraventricular tachycardia causes episodes of a pounding heartbeat that start and stop suddenly.
- Ventricular fibrillation. Rapid, chaotic electrical signals cause the lower heart chambers to quiver instead of squeezing in a coordinated way. This serious problem can lead to death if a regular heart rhythm isn't restored within minutes. Most people with ventricular fibrillation have an underlying heart disease or had a serious injury.
- Ventricular tachycardia. This rapid, irregular heart rate starts with faulty electrical signals in the lower heart chambers, called the ventricles. The rapid heart rate doesn't let the ventricles properly fill with blood. So the heart may not be able to pump enough blood to the body. Ventricular tachycardia may not cause serious problems in people with otherwise healthy hearts. In those with heart disease, ventricular tachycardia can be an emergency that needs immediate medical care.
Slow heartbeat, called bradycardia
A heart rate below 60 beats a minute is considered bradycardia. But a low resting heart rate doesn't always mean there's a problem. If you're physically fit, your heart may be able to pump enough blood to the body with less than 60 beats a minute.
If you have a slow heart rate and your heart isn't pumping enough blood, you may have a type of bradycardia. Types of bradycardias include:
- Sick sinus syndrome. The sinus node sets the pace of the heart. If the node doesn't work properly, the heart rate may switch between too slow and too fast. Sick sinus syndrome can be caused by scarring near the sinus node that slows, disrupts or blocks heartbeat signals. The condition is most common among older adults.
- Conduction block. A block of the heart's electrical pathways can cause the signals that trigger the heartbeats to slow down or stop. Some blocks may cause no symptoms. Others may cause skipped beats or slowed heartbeats.
Premature heartbeats
Premature heartbeats are extra beats that occur one at a time, sometimes in patterns that alternate with a regular heartbeat. If the extra beats come from the top chamber of the heart, they are called premature atrial contractions (PACs). If they come from the bottom chamber, they are called premature ventricular contractions (PVCs).
A premature heartbeat may feel like your heart skipped a beat. These extra beats are generally not a concern. They rarely mean you have a more serious condition. Still, a premature beat can trigger a longer lasting arrhythmia, especially in people with heart disease. Occasionally, having very frequent premature ventricular beats may lead to a weak heart.
Premature heartbeats may occur when resting. Stress, heavy exercise and the use of stimulants, such as caffeine or nicotine, also may cause premature heartbeats.
Symptoms
A heart arrhythmia may not cause any symptoms. The irregular heartbeat may be noticed during a health checkup for another reason.
Symptoms of an arrhythmia may include:
- A fluttering, pounding or racing feeling in the chest.
- A fast heartbeat.
- A slow heartbeat.
- Chest pain.
- Shortness of breath.
Other symptoms may include:
- Anxiety.
- Feeling very tired.
- Lightheadedness or dizziness.
- Sweating.
- Fainting or almost fainting.
When to see a doctor
If you feel like your heart is beating too fast or too slow, or it's skipping a beat, make an appointment for a health checkup. You may be told to see a doctor trained in heart diseases, called a cardiologist.
Get emergency medical care if you have these heart symptoms:
- Chest pain.
- Shortness of breath.
- Fainting.
Always call 911 or your local emergency number if you think you might be having a heart attack.
A type of arrhythmia called ventricular fibrillation can cause a dramatic drop in blood pressure. This can cause the person to fall to the ground within seconds, also called collapse. Soon the person's breathing and pulse will stop. Ventricular fibrillation is an emergency that needs immediate medical help. It's the most frequent cause of sudden cardiac death.
If this happens, follow these steps:
- Call 911 or your local emergency number.
- If there's no one nearby trained in cardiopulmonary resuscitation (CPR), provide hands-only CPR. Push hard and fast on the center of the chest. Do 100 to 120 compressions a minute until medical help arrives. You do not need to breathe into the person's mouth.
- CPR helps keep blood flowing to the organs until an electrical shock can be given with an automated external defibrillator (AED). An AED is a device that delivers a shock to restart the heart.
- If an AED is available nearby, have someone get the device and follow the instructions. No training is required to use it. The device tells you what to do. It's programmed to allow a shock only when appropriate.
Causes
To understand the cause of heart arrhythmias, it may help to know how the heart works.
How does the heart beat?
The typical heart has four chambers.
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
The heart's electrical system controls the heartbeat. The heart's electrical signals start in a group of cells at the top of the heart called the sinus node. They pass through a pathway between the upper and lower heart chambers called the atrioventricular (AV) node. The movement of the signals causes the heart to squeeze and pump blood.
In a healthy heart, this heart signaling process usually goes smoothly, resulting in a resting heart rate of 60 to 100 beats a minute.
But some things can change how electrical signals travel through the heart and cause arrhythmias. They include:
- A heart attack or scarring from a previous heart attack.
- Blocked arteries in the heart, called coronary artery disease.
- Changes to the heart's structure, such as from cardiomyopathy.
- Diabetes.
- High blood pressure.
- Infection with COVID-19.
- Overactive or underactive thyroid gland.
- Sleep apnea.
- Some medicines, including those used to treat colds and allergies.
- Drinking too much alcohol or caffeine.
- Illegal drug use or drug misuse.
- Genetics.
- Smoking.
- Stress or anxiety.
Risk factors
Things that may increase the risk of heart arrhythmias include:
- Coronary artery disease, other heart problems and previous heart surgery. Narrowed heart arteries, a heart attack, heart valve disease, prior heart surgery, heart failure, cardiomyopathy and other heart damage are risk factors for almost any kind of arrhythmia.
- High blood pressure. This condition increases the risk of developing coronary artery disease. It also may cause the walls of the left lower heart chamber to become stiff and thick, which can change how electrical signals travel through the heart.
- Heart problems present at birth. Also called congenital heart defects, some of these problems may affect the heart rate and rhythm.
- Thyroid disease. Having an overactive or underactive thyroid gland can raise the risk of irregular heartbeats.
- Obstructive sleep apnea. This condition causes pauses in breathing during sleep. It can lead to a slow heartbeat and irregular heartbeats, including atrial fibrillation.
- Electrolyte imbalance. Substances in the blood called electrolytes help trigger and send electrical signals in the heart. Potassium, sodium, calcium and magnesium are examples of electrolytes. If the body's electrolytes are too low or too high, it may interfere with heart signaling and lead to irregular heartbeats.
- Some medicines and supplements. Some prescription medicines and certain cough and cold treatments can cause arrhythmias.
- Excessive alcohol use. Drinking too much alcohol can affect electrical signaling in the heart. This can increase the chance of developing atrial fibrillation.
- Caffeine, nicotine or illegal drug use. Stimulants can cause the heart to beat faster and may lead to the development of more-serious arrhythmias. Illegal drugs, such as amphetamines and cocaine, may greatly affect the heart. Some may cause sudden death due to ventricular fibrillation.
Complications
Complications depend on the type of heart arrhythmia. Possible complications of heart arrhythmias include:
- Blood clots, which can lead to stroke.
- Heart failure.
- Sudden cardiac death.
Blood-thinning medicines can lower the risk of stroke related to atrial fibrillation and other heart arrhythmias. If you have a heart arrhythmia, ask a healthcare professional if you need to take a blood thinner.
If an arrhythmia is causing heart failure symptoms, treatment to control the heart rate may help the heart work better.
Prevention
Lifestyle changes used to manage heart disease may help prevent heart arrhythmias. Try these heart-healthy tips:
- Don't smoke.
- Eat a diet that's low in salt and saturated fat.
- Exercise at least 30 minutes a day on most days of the week.
- Maintain a healthy weight.
- Reduce and manage stress.
- Control high blood pressure, high cholesterol and diabetes.
- Get good sleep. Adults should aim for 7 to 9 hours daily.
- Limit or avoid caffeine and alcohol.
Oct. 13, 2023