Diagnosis
Kidney biopsy
Kidney biopsy
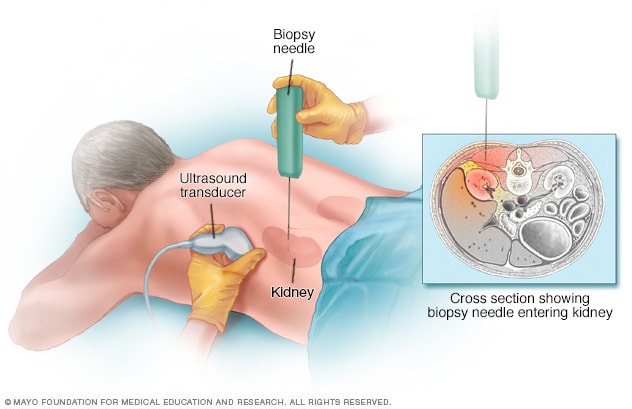
During a kidney biopsy, a healthcare professional uses a needle to remove a small sample of kidney tissue for lab testing. The biopsy needle is put through the skin to the kidney. The procedure often uses an imaging device, such as an ultrasound transducer, to guide the needle.
Glomerulonephritis may be identified with tests if you have an acute illness or during routine testing during a wellness visit or an appointment managing a chronic disease, such as diabetes. Tests to assess your kidney function and make a diagnosis of glomerulonephritis include:
- Urine test. A urinalysis can reveal signs of poor kidney function, such as red blood cells and proteins that should not be in urine or white blood cells that are a sign of inflammation. There also may be a lack of the expected levels of waste products.
- Blood tests. Analysis of blood samples can reveal higher than expected levels of waste products in the bloodstream, the presence of antibodies that may indicate an autoimmune disorder, bacterial or viral infection, or blood sugar levels indicating diabetes.
- Imaging tests. If your doctor detects evidence of kidney disease, he or she may recommend imaging tests that may show an irregularity in the shape or size of the kidney. These tests may be an X-ray, an ultrasound exam or a CT scan.
- Kidney biopsy. This procedure involves using a special needle to extract small pieces of kidney tissue to look at under a microscope. A biopsy is used to confirm a diagnosis and to assess the degree and nature of tissue damage.
More Information
Treatment
Treatment of glomerulonephritis and your outcome depend on:
- Whether you have an acute or chronic form of the disease.
- The underlying cause.
- The type and severity of your signs and symptoms.
Some cases of acute glomerulonephritis, especially those that follow an infection with streptococcal bacteria, might improve on their own and require no treatment. If there's an underlying cause — such as high blood pressure, an infection or an autoimmune disease — treatment will be directed to the underlying cause.
In general, the goal of treatment is to protect your kidneys from further damage and to preserve kidney function.
Therapies for associated kidney failure
Kidney failure is the loss of 85% or more of kidney function. Acute kidney failure due to infection-related glomerulonephritis is treated with dialysis. Dialysis uses a device that works like an artificial, external kidney that filters your blood.
End-stage kidney disease is chronic kidney disease that can only be managed by regular kidney dialysis or a kidney transplant.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
If you have kidney disease, your doctor might recommend certain lifestyle changes:
- Lower your salt intake to prevent or minimize fluid retention, swelling and hypertension.
- Consume less protein and potassium to slow the buildup of wastes in your blood.
- Maintain a healthy weight.
- Take your medications as directed by your health care provider.
- Control your blood sugar level if you have diabetes.
- Quit smoking.
Coping and support
Living with a chronic illness can tax your emotional resources. If you have chronic glomerulonephritis or chronic kidney failure, you might benefit from joining a support group. A support group can provide both sympathetic listening and useful information.
To find a support group, ask your doctor for a recommendation or contact the National Kidney Foundation to find the chapter nearest you.
Preparing for your appointment
You'll likely start by seeing your primary care provider. If lab tests reveal that you have kidney damage, you might be referred to a doctor who specializes in kidney problems (nephrologist).
What you can do
To get ready for your appointment, ask if there's anything you need to do ahead of time, such as limit what you eat and drink. Then make a list of items you'll likely need to discuss with your health care provider:
- Your symptoms, including any that seem unrelated to your kidneys or urinary function, and when they began.
- All your medications and doses, including vitamins or other supplements that you take.
- Your key medical history, including any other medical conditions and family medical history.
Take a family member or friend along, if possible, to help you remember the information you're given.
When you have follow-up appointments after a diagnosis of glomerulonephritis, you may want to ask the following questions:
- How well are my kidneys functioning? Has the function changed since the previous exam?
- When should I schedule lab work or another appointment?
- Will I need dialysis?
- What help can I get to manage related conditions, such as support with diet planning or exercise?
- What do I do if I miss a dosage of a prescription?
- When should I call for an appointment or get urgent care?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Feb. 24, 2024