Diagnosis
Coronary artery disease FAQs
Mayo Clinic cardiologist Stephen Kopecky, M.D., answers the most frequently asked questions about coronary artery disease (CAD).
Hi, I'm Dr. Steve Kopecky, a cardiologist at Mayo Clinic. And I'm here to answer some of the important questions you may have about coronary artery disease.
Many small changes can lead to great benefit over time. Remember that nothing you do to improve your health is ever too little. And nothing you do to improve your health is ever too late.
Cholesterol is always involved in the initiation of the narrowing of the arteries to the heart. And every plaque or narrowing of your arteries contains cholesterol. It is essential to control the cholesterol in order to optimally lower your chance of a heart attack.
Yes. All the studies that have shown regression of arterial narrowing have done three things. First, take care of the obvious factors like high blood pressure, smoking and high cholesterol. Second, address diet and physical activity. And third, help patients manage stress.
No. Half of the time, the first symptom a person has of coronary artery disease is actually a heart attack. And half of these heart attacks are fatal. So overall, for one out of four people, the first symptom is what we term sudden cardiac death.
No. Studies have shown that even if your cholesterol is well control with medicines, if you do not eat a healthy diet, your heart attack, stroke, and death rate is not significantly reduced.
Yes. Since your heart beats one hundred thousand times a day, even mild elevations of blood pressure above 130 over 80 can cause significant health problems, including heart attacks, strokes and heart failure.
I tell people they have a new part-time job called Your Health. In part of this is knowing what medicines you're on, what doses you're taking and why you're taking these medicines. Also very helpful, check your blood pressure regularly. Check your weight regularly at home. If any questions arise about your health, put them in your smartphone, so you'll have them the next time you have your visit with your doctor. Never hesitate to ask your medical team any questions or concerns you have. Being informed makes all the difference. Thanks for your time and we wish you well.
To diagnose coronary artery disease, a healthcare professional examines you. You are usually asked questions about your medical history and any symptoms. If you have symptoms of coronary artery disease such as chest pain or shortness of breath, tests may be done to check your overall health.
Tests
Tests to help diagnose or watch coronary artery disease include:
- Blood tests. Blood tests can check blood sugar and cholesterol levels. A high-sensitivity C-reactive protein (CRP) test checks for a protein linked to inflammation of the arteries.
- Electrocardiogram (ECG or EKG). This quick test checks the electrical activity of the heart. It shows how the heart is beating. Sticky patches called electrodes attach to the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which prints or displays the test results. The ECG signal patterns can show if you had or are having a heart attack.
- Echocardiogram. This test uses sound waves to show blood flow through the heart. Parts of the heart that move weakly may be caused by a lack of oxygen or a heart attack. This may be a sign of coronary artery disease or other conditions.
- Exercise stress test. If your symptoms usually occur during exercise, your healthcare professional may recommend this test. You walk on a treadmill or ride a stationary bike while your heart is checked. Because exercise makes the heart pump harder and faster than it does during most daily activities, an exercise stress test can show heart problems that might otherwise be missed. If you can't exercise, you may be given a medicine that affects the heart like exercise does. Sometimes an echocardiogram is done during an exercise stress test.
- Nuclear stress test. This test shows how blood moves to the heart at rest and during activity. It uses a small amount of radioactive material, called a tracer or radiotracer. The substance is given by IV. An imaging machine takes pictures of how the tracer moves through the heart arteries. This helps find areas of poor blood flow or heart damage.
- Heart CT scan. A CT scan of the heart can show calcium deposits and blockages in the heart arteries. Calcium deposits can narrow the arteries. Sometimes dye is given by IV during this test. The dye helps create detailed pictures of the heart arteries. If dye is used, the test is called a CT coronary angiogram.
- Cardiac catheterization and angiogram. This test can see blockages in the heart arteries. A doctor places a long, thin flexible tube called a catheter in a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video. Heart treatments may be done during this test.
More Information
Treatment
Treatment for coronary artery disease may include:
- Lifestyle changes such as not smoking, eating healthy and exercising more.
- Medicines.
- Heart procedure or heart surgery.
Medications
Many medicines are available to treat coronary artery disease, including:
- Cholesterol medicine. Your healthcare professional might recommend this type of medicine to lower "bad" LDL cholesterol and reduce plaque buildup in the arteries. Such medicines include statins, niacin, fibrates and bile acid sequestrants.
-
Aspirin. Aspirin helps thin the blood and prevent blood clots. Daily low-dose aspirin therapy may be recommended for the primary prevention of heart attack or stroke in some people.
Daily use of aspirin can have serious side effects, including bleeding in the stomach and intestines. Don't start taking a daily aspirin without talking to your healthcare team.
- Beta blockers. These medicines slow the heartbeat and lower blood pressure. If you've had a heart attack, beta blockers may reduce the risk of future heart attacks.
- Calcium channel blockers. One of these medicines may be suggested if you can't take beta blockers or beta blockers don't work for you. Calcium channel blockers can help reduce chest pain.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs). These medicines lower blood pressure. They may help keep coronary artery disease from getting worse.
- Nitroglycerin. This medicine widens the heart arteries. It can help control or reduce chest pain. Nitroglycerin is available as a pill, spray or patch.
- Ranolazine. This medicine may help people with long-term chest pain. It may be prescribed with or instead of a beta blocker.
Surgeries or other procedures
Coronary artery stent

Coronary artery stent
To place a coronary artery stent, a balloon on the tip of the catheter is inflated to widen the blocked artery (A). Then a metal mesh stent is placed (B). The stent helps hold the artery open so blood can flow through it (C).
Coronary artery bypass surgery
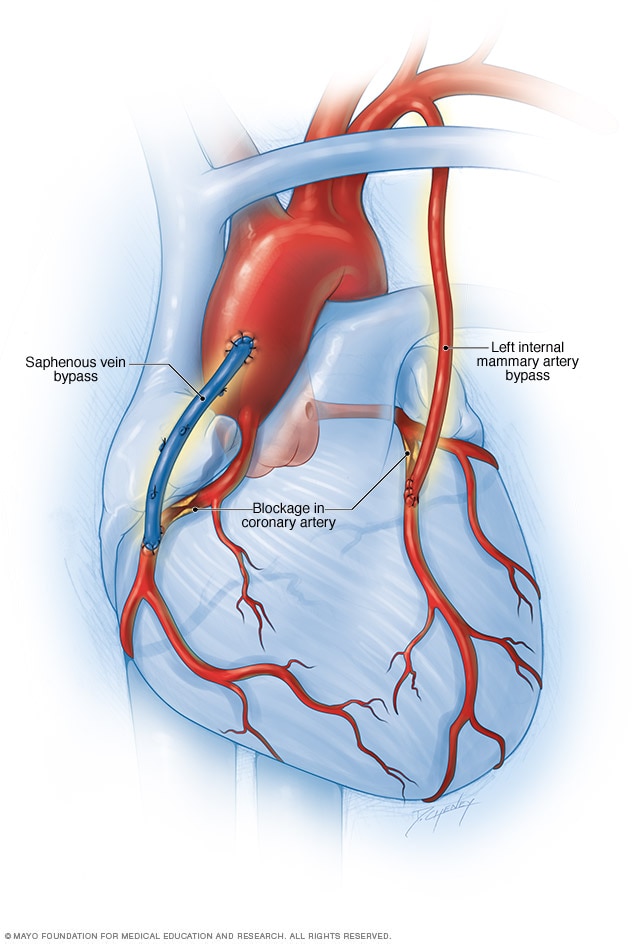
Coronary artery bypass surgery
Coronary artery bypass surgery creates a new path for blood to flow to the heart. A healthy blood vessel from another part of the body is used to redirect blood around a blocked area of an artery. Usually the blood vessel is taken from an artery in the chest, called the internal mammary artery. Sometimes it's taken from a leg vein, called the saphenus vein.
Surgery may be done to fix a blocked artery and improve blood flow. Surgeries or procedures for coronary artery disease may include:
- Coronary angioplasty and stent placement. This treatment opens clogged blood vessels in the heart. A tiny balloon on a thin tube, called a catheter, is used to widen a clogged artery and improve blood flow. A small wire mesh tube called a stent may be placed to keep the artery open. Most stents are coated with medicine that helps keep the artery open. This treatment also is called percutaneous coronary intervention.
- Coronary artery bypass graft (CABG) surgery. This is a type of open-heart surgery. During CABG, a surgeon takes a vein or artery from somewhere else in the body. The surgeon uses the blood vessel to create a new path for blood to go around a blocked or narrowed heart artery. The surgery increases blood flow to the heart.
If you've had coronary artery bypass surgery, your healthcare professional may suggest cardiac rehabilitation. This is a program of education, counseling and exercise training that's designed to help improve your health after heart surgery.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
Omega-3 fatty acids are a type of unsaturated fatty acid. It's thought that they can lower inflammation throughout the body. Inflammation has been linked to coronary artery disease. However, the reasons for and against omega-3 fatty acids for heart disease continue to be studied.
Sources of omega-3 fatty acids include:
- Fish and fish oil. Fish and fish oil are the most effective sources of omega-3 fatty acids. Fatty fish — such as salmon, herring and light canned tuna — have the most omega-3 fatty acids. Fish oil supplements may offer benefit, but the evidence is strongest for eating fish.
- Flax and flaxseed oil. Flax and flaxseed oil contain a type of omega-3 fatty acid called alpha-linolenic acid (ALA). ALA contains smaller amounts of omega-3 fatty acids than do fish and fish oil. ALA may help lower cholesterol and improve heart health. But research is mixed. Some studies haven't found flax and flaxseed oil to be as effective as fish. Flaxseed also contains a lot of fiber, which has various health benefits.
- Other oils. Alpha-linolenic acid (ALA) also can be found in canola oil, soybeans and soybean oil.
Other supplements and food items may help lower blood pressure or cholesterol — two risk factors for coronary artery disease. Some that may work are:
- Barley.
- Psyllium, a type of fiber.
- Oats, a type of fiber that includes beta-glucans and is found in oatmeal and whole oats.
- Garlic.
- Plant sterols, found in supplements and some margarines, such as Promise, Smart Balance and Benecol.
Always talk to a healthcare professional before taking herbs, supplements or medicines bought without a prescription.
Lifestyle and home remedies
Making certain lifestyle changes can help keep the arteries healthy and can prevent or slow coronary artery disease. Try these heart-healthy tips:
- Don't smoke or use tobacco. Smoking is a major risk factor for coronary artery disease. Nicotine tightens blood vessels and forces the heart to work harder. Not smoking is one of the best ways to lower the risk of a heart attack. If you need help quitting, talk to your healthcare team.
- Eat heart-healthy foods. Choose plenty of fruits, vegetables and whole grains. Limit sugar, salt and saturated fats. Eating one or two servings of fish a week also may help keep the heart healthy.
- Get regular exercise. Exercise helps manage weight and control diabetes, cholesterol and blood pressure — all risk factors for coronary artery disease. Try to get 30 to 60 minutes of physical activity most days of the week. Ask your healthcare team what amount and type of exercise is best for you.
- Keep a healthy weight. Being overweight increases the risk of coronary artery disease. Losing even a small amount of weight can help reduce risk factors for coronary artery disease. Ask your healthcare team what the best weight is for you.
- Control blood pressure. Adults should get their blood pressure checked by a healthcare professional at least every two years. You may need to have checks more often if you have a history of high blood pressure. Ask your health professional what blood pressure goal is best for you.
- Get your cholesterol checked. Ask your healthcare team how often you need a cholesterol test. Lifestyle changes and medicines may be recommended to control cholesterol.
- Check your blood sugar. If you have diabetes, carefully managing your blood sugar can help reduce the risk of coronary artery disease.
- Avoid or limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Get good sleep. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce stress.
Regular health checkups also are important. Some of the main risk factors for coronary artery disease — high cholesterol, high blood pressure and diabetes — have no symptoms in the early stages. Early detection and treatment can help you keep your heart healthy. Also ask about recommended vaccines, such as a yearly flu vaccine.
Prevention
The lifestyle habits used to treat coronary artery disease also can help prevent it. A healthy lifestyle can help keep the arteries strong and clear of blockages. To improve heart health, follow these tips:
- Do not smoke or use tobacco.
- Limit or do not drink alcohol.
- Control blood pressure, cholesterol and diabetes.
- Exercise and stay active.
- Maintain a healthy weight.
- Eat a low-fat, low-salt diet that's rich in fruits, vegetables and whole grains.
- Reduce and manage stress.
- Get 7 to 9 hours of sleep daily.
Preparing for your appointment
If you have symptoms of coronary artery disease or any risk factors, make an appointment for a health checkup. You may be sent to a doctor trained in heart diseases, called a cardiologist.
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet. For example, you may be told not to eat or drink for a few hours before a cholesterol test.
- Write down any symptoms you're having, including any that may seem unrelated to coronary artery disease.
- Write down your medical information, including other conditions you have and any family history of heart disease.
- Bring a list of medicines with you to your appointment. Include doses.
- Ask a family member or friend to go with you to the appointment, if possible. An extra person can help you remember details from the appointment..
- Write down questions to ask your healthcare team.
Questions to ask your healthcare professional at your first appointment include:
- What is causing my symptoms?
- What tests do I need?
- Should I see a specialist?
- Do I need to change my activity or diet while I wait for my next appointment?
- When should I call 911 or emergency medical help for my symptoms?
If you're sent to a cardiologist for coronary artery disease, you may want to ask these questions:
- What is my risk of long-term complications from coronary artery disease?
- What treatment do you recommend?
- If I need medicine, what are the possible side effects?
- Do I need surgery? Why or why not?
- What diet and lifestyle changes should I make?
- How often do I need follow-up visits?
- I have other health conditions. How can I best manage these conditions together?
Don't hesitate to ask additional questions.
What to expect from your doctor
A healthcare professional who sees you for coronary artery disease may ask:
- What are your symptoms?
- When did you begin having symptoms?
- Have the symptoms gotten worse over time?
- Do you have chest pain or difficulty breathing?
- If so, what does the chest pain feel like?
- Does exercise or activity make the symptoms worse?
- Does anyone in your family have a heart condition or high blood pressure?
- Have you been diagnosed with other health conditions?
- What medicines do you take?
- How much do you exercise in a typical week?
- What's your usual daily diet?
- Do you or did you smoke? How much? If you quit, when?
- Do you drink alcohol? How much?
What you can do in the meantime
It's never too early to make healthy lifestyle changes, such as quitting smoking, eating healthy foods and getting more exercise. These habits protect against coronary artery disease and its complications, including heart attack and stroke.