Overview
Brain AVM
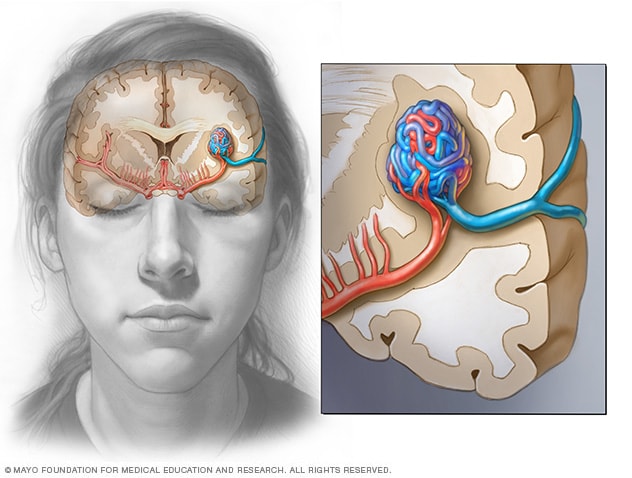
Brain AVM
In a brain AVM, blood passes directly from the arteries to the veins via tangled vessels. This disrupts the typical process of how blood circulates through the brain.
Blood vessels in brain AVM
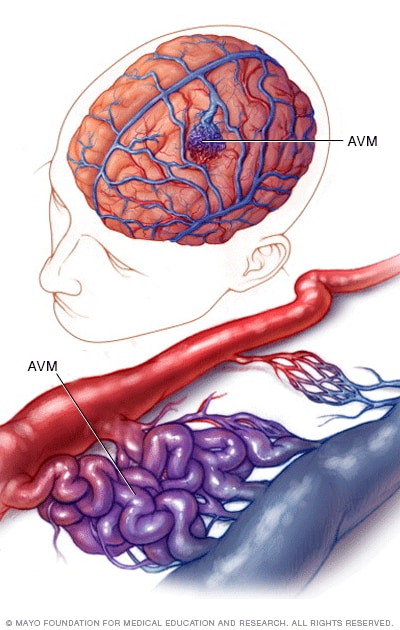
Blood vessels in brain AVM
In a brain arteriovenous malformation, blood passes directly from arteries to veins through a tangle of blood vessels.
A brain arteriovenous malformation (AVM) is a tangle of blood vessels that creates irregular connections between arteries and veins in the brain.
Arteries take oxygen-rich blood from the heart to the brain. Veins carry oxygen-depleted blood back to the lungs and heart. A brain AVM disrupts this vital process.
An arteriovenous malformation can develop anywhere in the body, but common locations include the brain and spinal cord. Overall, brain AVMs are rare.
The cause of brain AVMs isn't clear. Most people who have them are born with them, but they can form later in life. Rarely, AVM can be a trait passed down in families.
Some people with brain AVMs experience symptoms such as headaches or seizures. A brain AVM may be found after a brain scan for another health issue. Sometimes a brain AVM is found after the blood vessels burst and bleed, known as a hemorrhage.
Once diagnosed, a brain AVM can be treated to prevent complications such as brain damage or stroke.
Products & Services
Symptoms
A brain arteriovenous malformation (AVM) may not cause any symptoms until the AVM bursts and bleeds, known as a hemorrhage. In about half of all brain AVMs, a hemorrhage is the first sign of the malformation.
But some people with brain AVMs may experience symptoms other than bleeding, such as:
- Seizures.
- Headaches or pain in one area of the head.
- Muscle weakness or numbness in one part of the body.
Some people may experience more-serious symptoms depending on the location of the AVM, including:
- A very bad headache.
- Weakness, numbness or paralysis.
- Vision loss.
- Trouble speaking.
- Confusion or not being able to understand others.
- Trouble with walking.
Symptoms of a brain AVM may begin at any age but usually appear between ages 10 and 40. Brain AVMs can damage brain tissue over time. The effects slowly build and often cause symptoms in early adulthood.
By middle age, however, brain AVMs tend to remain stable and are less likely to cause symptoms.
When to see a doctor
Get medical care right away if you notice any symptoms of a brain AVM, such as seizures, headaches or other symptoms. A bleeding brain AVM is dangerous and requires emergency medical care.
Causes
AVM blood flow
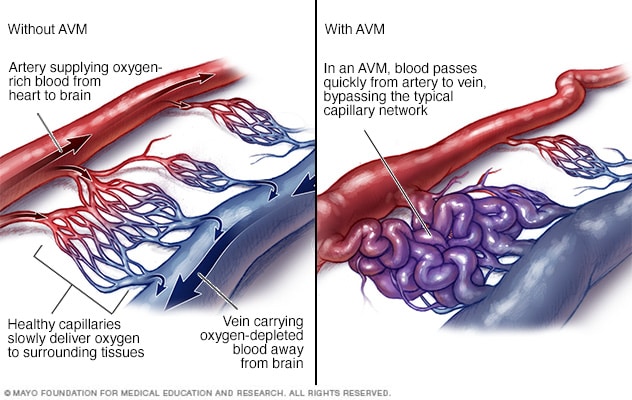
AVM blood flow
In an arteriovenous malformation, also known as an AVM, blood passes quickly from an artery to a vein, disrupting the usual blood flow and depriving the surrounding tissues of oxygen.
The cause of brain arteriovenous malformations (AVMs) is not known. Researchers believe most brain AVMs are present at birth and form during a baby's growth in the womb. But brain AVMs can happen later in life as well.
Brain AVMs are seen in some people who have hereditary hemorrhagic telangiectasia (HHT). HHT also is known as Osler-Weber-Rendu syndrome. HHT affects the way blood vessels form in several areas of the body, including the brain.
Typically, the heart sends oxygen-rich blood to the brain through arteries. The arteries slow blood flow by passing the blood through a series of smaller and smaller blood vessels. The smallest blood vessels are called capillaries. The capillaries slowly deliver oxygen through their thin, porous walls to the surrounding brain tissue.
The oxygen-depleted blood passes into small blood vessels and then into larger veins. The veins return the blood to the heart and lungs to get more oxygen.
The arteries and veins in an AVM lack this supporting network of smaller blood vessels and capillaries. Instead, blood flows quickly and directly from the arteries to the veins. When this happens, surrounding brain tissue doesn't receive the oxygen it needs.
Risk factors
Anyone can be born with a brain arteriovenous malformation (AVM), but these factors may raise the risk:
- Being male. Brain AVMs are more common in men.
- Having a family history. Rarely, brain AVMs occur in families, but it's not clear if there's a certain genetic risk factor. It's also possible to inherit other medical conditions that increase the risk of brain AVMs, such as hereditary hemorrhagic telangiectasia (HHT).
Complications
Intracerebral hemorrhage
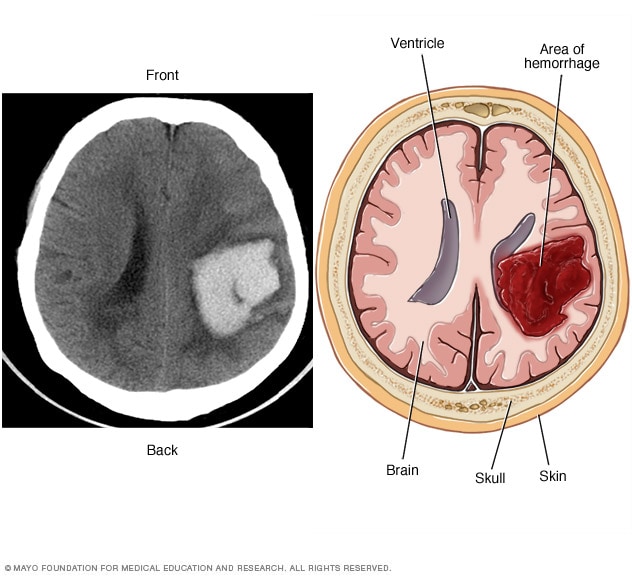
Intracerebral hemorrhage
A brain AVM may cause bleeding in the brain, known as a hemorrhage. Bleeding can damage the surrounding brain tissue. The CT scan on the left and the illustration on the right show an intracerebral hemorrhage.
Complications of a brain arteriovenous malformation (AVM) include:
-
Bleeding in the brain. A brain AVM puts extreme pressure on the walls of the affected arteries and veins. The pressure causes the arteries and veins to become thin or weak. This may result in the AVM breaking open and bleeding into the brain, known as a hemorrhage.
This risk of a brain AVM bleeding ranges from around 2% to 3% each year. The risk of bleeding may be higher for certain types of AVM. Risk also may be higher in people who have had a brain AVM bleed in the past.
Although studies haven't found that pregnancy increases the risk of hemorrhage in people with a brain AVM, more research is needed.
Some hemorrhages associated with brain AVMs aren't detected because they cause no major symptoms. However, potentially dangerous bleeding can occur.
Brain AVMs account for about 2% of all hemorrhagic strokes each year. In children and young adults who experience brain hemorrhage, brain AVMs are often the cause.
-
Reduced oxygen to brain tissue. With a brain AVM, blood doesn't flow through the network of small blood vessels called capillaries. Instead, it flows directly from arteries to veins. Blood rushes quickly because it isn't slowed by the smaller blood vessels.
Surrounding brain tissue can't easily absorb oxygen from the fast-flowing blood. Without enough oxygen, brain tissues weaken or may die off completely. This results in stroke-like symptoms, such as trouble speaking, weakness, numbness, vision loss or trouble staying steady.
- Thin or weak blood vessels. An AVM puts extreme pressure on the thin and weak walls of the blood vessels. A bulge in a blood vessel wall, known as an aneurysm, may form. The aneurysm may be at risk of bursting.
-
Brain damage. The body may use more arteries to supply blood to the fast-flowing brain AVM. As a result, some AVMs may get bigger and displace or compress portions of the brain. This may prevent protective fluids from flowing freely around the brain.
If fluid builds up, it can push brain tissue against the skull.
One type of brain AVM that involves a major blood vessel called the vein of Galen causes serious complications in babies. Symptoms are present at birth or appear soon after birth. This type of brain AVM causes fluid to build up in the brain and the head to swell. Swollen veins may be seen on the scalp, and seizures may occur. Children with this type of brain AVM can have a failure to thrive and congestive heart failure.