Overview
Anthrax is a rare but serious illness caused by a spore-forming bacterium, Bacillus anthracis. Anthrax mainly affects livestock and wild game. Humans can become infected through direct or indirect contact with sick animals.
There's no evidence that anthrax is transmitted from person to person, but it's possible that anthrax skin lesions may be contagious through direct contact or through contact with a contaminated object (fomite). Usually, anthrax bacteria enter the body through a wound in the skin. You can also become infected by eating contaminated meat or inhaling the spores.
Signs and symptoms, which depend on how you're infected, can include skin sores, vomiting and shock. Prompt treatment with antibiotics can cure most anthrax infections. Inhaled anthrax is more difficult to treat and can be fatal.
Anthrax is very rare in the developed world. However, the illness remains a concern because the bacteria have been used in bioterrorism attacks in the United States.
Symptoms
There are four common routes of anthrax infection, each with different signs and symptoms. In most cases, symptoms develop within six days of exposure to the bacteria. However, it's possible for inhalation anthrax symptoms to take more than six weeks to appear.
Cutaneous anthrax
A skin-related (cutaneous) anthrax infection enters your body through your skin, usually through a cut or other sore. It's by far the most common route of the disease. It's also the mildest. With appropriate treatment, cutaneous anthrax is seldom fatal. Signs and symptoms include:
- A raised, itchy bump resembling an insect bite that quickly develops into a painless sore with a black center
- Swelling in the sore and nearby lymph glands
- Sometimes, flu-like symptoms including fever and headache

Cutaneous anthrax
You can contract anthrax when spores penetrate your skin, usually through an open wound. The infection begins as a raised, sometimes itchy, bump resembling an insect bite. But within a day or two, the bump develops into an open, usually painless sore with a black center.
Gastrointestinal anthrax
A gastrointestinal anthrax infection results from eating undercooked meat from an infected animal. It can affect your gastrointestinal tract from your throat to your colon. Signs and symptoms include:
- Nausea
- Vomiting
- Abdominal pain
- Headache
- Loss of appetite
- Fever
- Severe, bloody diarrhea in the later stages of the disease
- Sore throat and difficulty swallowing
- Swollen neck
Inhalation anthrax
Inhalation anthrax develops when you breathe in anthrax spores. It's the most deadly form of the disease, and is often fatal, even with treatment. Initial signs and symptoms include:
- Flu-like symptoms for a few hours or days, such as sore throat, mild fever, fatigue and muscle aches
- Mild chest discomfort
- Shortness of breath
- Nausea
- Coughing up blood
- Painful swallowing
- High fever
- Trouble breathing
- Shock — an acute medical condition involving collapse of the circulatory system
- Meningitis
Inhalation anthrax
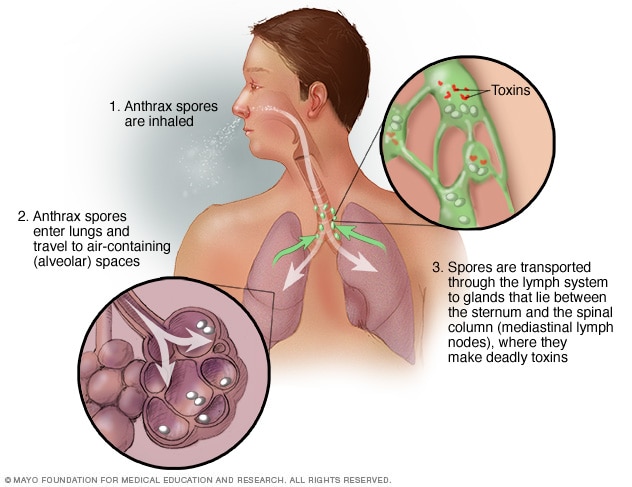
This illustration shows how the spores that cause inhalation anthrax — the most deadly form of anthrax infection — enter and affect the body.
Injection anthrax
This recently identified route of anthrax infection has so far been reported only in Europe. It's contracted through injecting illegal drugs. Initial signs and symptoms include:
- Redness at the area of injection (without an area that changes to black)
- Significant swelling
- Shock
- Multiple organ failure
- Meningitis
When to see a doctor
Many common illnesses start with symptoms that resemble the flu. The chances that your sore throat and aching muscles are due to anthrax are extremely small.
If you think you may have been exposed — for example, if you work in an environment where anthrax is likely to occur — see a doctor immediately for evaluation and care. If you develop signs and symptoms of the disorder after exposure to animals or animal products in parts of the world where anthrax is common, seek prompt medical attention. Early diagnosis and treatment are crucial.
Causes
Anthrax spores are formed by anthrax bacteria that occur naturally in soil in most parts of the world. The spores can remain dormant for years until they find their way into a host. Common hosts for anthrax include wild or domestic livestock, such as sheep, cattle, horses and goats.
Although rare in the United States, anthrax is still common throughout the developing world, in places such as Central America and South America, sub-Saharan Africa, Central Asia and southwestern Asia, southern Europe and Eastern Europe, and the Caribbean.
Most human cases of anthrax occur as a result of exposure to infected animals or their meat or hides. In the United States, a few people have developed anthrax while making traditional African drums from the skins of infected animals.
One of the few known instances of nonanimal transmission was a bioterrorism attack that occurred in the United States in 2001. Twenty-two people developed anthrax after being exposed to spores sent through the mail, and five of those infected died.
More recently, in two separate outbreaks, heroin users in Europe contracted anthrax through injecting illegal drugs. A total of 40 people died. Heroin sold in Europe likely comes from areas where naturally occurring anthrax is more common.
Risk factors
To contract anthrax, you must come in direct contact with anthrax spores. This is more likely if you:
- Are in the military and deployed to an area with a high risk of exposure to anthrax
- Work with anthrax in a laboratory setting
- Handle animal skins, furs or wool from areas with a high incidence of anthrax
- Work in veterinary medicine, especially if you deal with livestock
- Handle or dress game animals — while anthrax is rare in the United States, there are occasional outbreaks in domestic cattle and wild animals such as deer
- Inject illegal drugs, such as heroin
Complications
The most serious complications of anthrax include:
- Your body being unable to respond to infection normally, leading to damage of multiple organ systems (sepsis)
- Inflammation of the membranes and fluid covering the brain and spinal cord, leading to massive bleeding (hemorrhagic meningitis) and death
Prevention
To prevent infection after being exposed to anthrax spores, the Centers for Disease Control and Prevention recommends:
- A 60-day treatment with antibiotics — ciprofloxacin, doxycycline and levofloxacin are approved for adults and children
- A three-dose series of anthrax vaccine
- In some cases, treatment with monoclonal antibodies — raxibacumab and obiltoxaximab
Anthrax vaccine
An anthrax vaccine is available for certain groups of people. The vaccine doesn't contain live bacteria and can't lead to infection. However, the vaccine can cause side effects, ranging from soreness at the injection site to more-serious allergic reactions.
The vaccine isn't intended for the general public. Instead, it's reserved for military personnel, scientists working with anthrax and people in other high-risk professions.
Avoiding infected animals
If you live or travel in a country where anthrax is common and herd animals aren't routinely vaccinated, avoid contact with livestock and animal skins as much as possible. Also avoid eating meat that hasn't been properly cooked.
Even in developed countries, it's important to handle any dead animal with care and to take precautions when working with or processing imported hides, fur or wool.