Aug. 06, 2021
Pathological acetabular fracture and superior migration of the femoral head

Pathological acetabular fracture and superior migration of the femoral head
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, an anteroposterior X-ray of the right hip reveals pathological acetabular fracture and superior migration of the femoral head into the acetabular defect.
Pathological acetabular fracture with loss of the posterior wall and posterior column

Pathological acetabular fracture with loss of the posterior wall and posterior column
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, an obturator oblique X-ray of the pelvis shows a pathological acetabular fracture with loss of the posterior wall and posterior column, and posterior subluxation of the right hip joint.
Superior and posterior acetabular bone loss
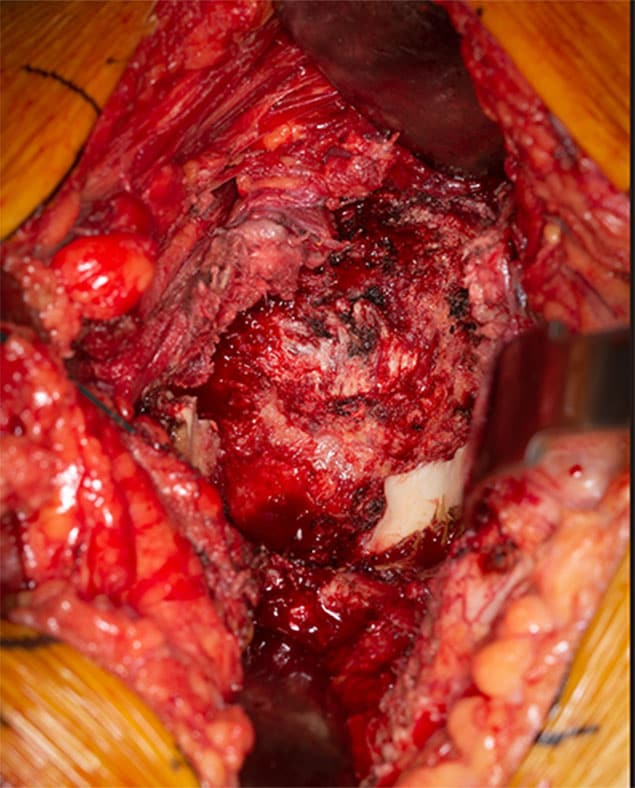
Superior and posterior acetabular bone loss
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, an intraoperative photo reveals severe superior and posterior acetabular bone loss. Only the inferior aspect of the acetabulum resembles native anatomical architecture.
Final reconstruction
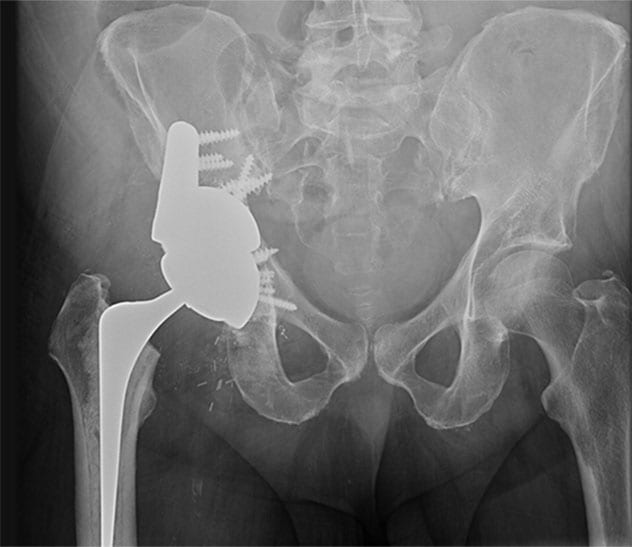
Final reconstruction
In a 56-year-old man with newly diagnosed metastatic lung carcinoma who presented at Mayo Clinic with excruciating right hip pain and who was unable to walk, a postoperative X-ray shows the final reconstruction. A highly porous tantalum augment was placed in the superior acetabular defect, followed by insertion of a highly porous tantalum revision shell obtaining a press fit between the augment and the remaining pubis and ischium. An additional buttress augment, also made of highly porous tantalum, was applied as additional fixation to the intact ilium. A cemented stem total hip arthroplasty was also used, due to plans for future radiation treatments. After surgery, the patient experienced significant pain relief and regained the ability to walk.
Joint reconstruction is particularly challenging in the setting of complex bony defects or radiation therapy. Mayo Clinic routinely uses 3D-printed models to optimize surgical outcomes for individual patients.
"This technology allows us to re-create a patient's bony defects and surgically correct them to restore joint function," says Cory G. Couch, M.D., an orthopedic surgeon at Mayo Clinic in Rochester, Minnesota, with fellowship training in orthopedic oncology and joint reconstruction. "We are able to model and fill in even very large bony defects created by tumors and tumor resections."
Mayo Clinic has the largest point-of-care additive manufacturing facility in the United States, staffed by radiologists and biomedical engineers. "They work in close conjunction with us," Dr. Couch says. "Complex joint reconstructions require multidisciplinary care from imaging experts and from radiation and medical oncologists, as well as orthopedic surgeons."
The 3D-printing technology is used in complex reconstructions of the knee, hip and pelvis for individuals with sarcoma or metastatic cancer. The technology also facilitates complex joint replacements associated with infection or the failure of a previous replacement joint.
The models are created using individual patients' CT scans or MRI or both and sterilizable materials. "In the operating room, we have the model on the table right next to the patient. That helps us to identify optimal implant placement or screw fixation," Dr. Couch says.
Arthroplasty and cancer care
Mayo Clinic commonly treats patients with bony defects due to cancer. Radiation and medical oncologists meet regularly with orthopedic surgeons to discuss patients and plan treatment. Surgical reconstruction of the hip or knee may precede or follow radiation treatment.
"We typically make these decisions based on the tumor type and location, but sometimes on a case-by-case basis," Dr. Couch says. "Sometimes having chemotherapy or radiation therapy upfront will reduce the size of the tumor, facilitate removal and optimize the maintenance of function."
Historically, patients having total hip arthroplasty after pelvic radiation experienced high rates of implant loosening when traditional uncemented acetabular components were used. But Mayo Clinic orthopedic researchers have found that 100% of modern, porous titanium components remained radiologically well fixed 10 years after implantation in patients having total hip arthroplasty after pelvic radiation. As described in the Journal of Arthroplasty, the mean overall pelvic radiation dose for the 33 patients in the study exceeded the radiation threshold for dose-related bone effects.
A separate study, described in The Journal of Bone and Joint Surgery, found that for patients with periacetabular metastatic disease, acetabular reconstruction using highly porous tantalum components provided a more durable construction and fewer complications compared with procedures using the cemented technique.
"Advances in medical care and radiotherapy mean that more cancer patients are living longer," Dr. Couch says. "Restoring patients' joints allows them to return to walking soon after surgery. The goal is for these patients to spend the remainder of their lives doing the things they want to do, relatively pain-free."
For more information
Wellings EP, et al. Contemporary porous titanium acetabular components for total hip arthroplasty after pelvic radiation. Journal of Arthroplasty. 2021;36:1714.
Houdek MT, et al. Comparison of porous tantalum acetabular implants and Harrington reconstruction for metastatic disease of the acetabulum. The Journal of Bone and Joint Surgery. 2020;102:1239.