Overview
Lymphedema refers to tissue swelling caused by an accumulation of protein-rich fluid that's usually drained through the body's lymphatic system. It most commonly affects the arms or legs, but can also occur in the chest wall, abdomen, neck and genitals.
Lymph nodes are an important part of your lymphatic system. Lymphedema can be caused by cancer treatments that remove or damage your lymph nodes. Any type of problem that blocks the drainage of lymph fluid can cause lymphedema.
Severe cases of lymphedema can affect the ability to move the affected limb, increase the risks of skin infections and sepsis, and can lead to skin changes and breakdown. Treatment may include compression bandages, massage, compression stockings, sequential pneumatic pumping, careful skin care and, rarely, surgery to remove swollen tissue or to create new drainage routes.
Products & Services
Symptoms
Parts of the immune system
Parts of the immune system
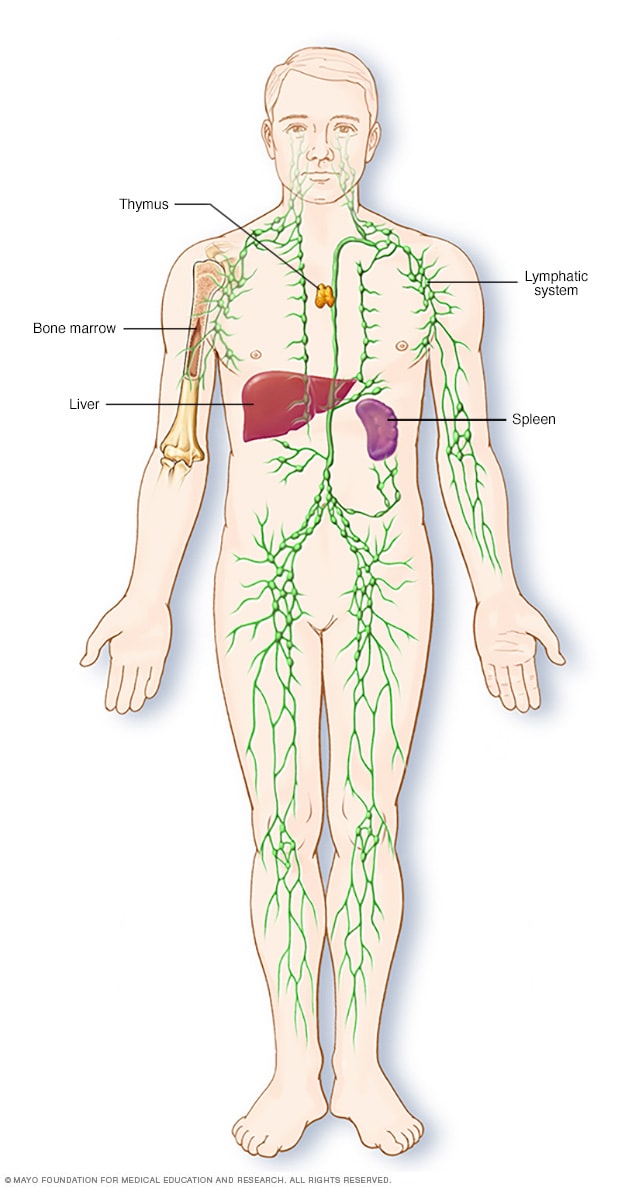
The lymphatic system is part of the body's immune system, which protects against infection and disease. The lymphatic system includes the spleen, thymus, lymph nodes and lymph channels, as well as the tonsils and adenoids.
Leg lymphedema

Leg lymphedema
Lymphedema is swelling in an arm or a leg. In rare circumstances, it affects both arms or both legs. It can also affect the chest wall and abdomen.
Lymphedema signs and symptoms include:
- Swelling of part or all of the arm or leg, including fingers or toes
- A feeling of heaviness or tightness
- Restricted range of motion
- Recurring infections
- Hardening and thickening of the skin (fibrosis)
Signs and symptoms can range from mild to severe. Lymphedema caused by cancer treatment may not occur until months or years after treatment.
When to see a doctor
Make an appointment with your doctor if you notice persistent swelling in your arm or leg. If you've already been diagnosed with lymphedema, see your doctor if there is a sudden dramatic increase in the size of the involved limb.
Causes
The lymphatic system is a network of vessels that carry protein-rich lymph fluid throughout the body. It's part of your immune system. Lymph nodes act as filters and contain cells that fight infection and cancer.
The lymph fluid is pushed through the lymph vessels by muscle contractions as you move through the tasks of your day and small pumps in the wall of the lymph vessels. Lymphedema occurs when the lymph vessels are not able to adequately drain lymph fluid, usually from an arm or leg.
The most common causes of lymphedema include:
- Cancer. If cancer cells block lymph vessels, lymphedema may result. For instance, a tumor growing near a lymph node or lymph vessel could enlarge enough to block the flow of the lymph fluid.
- Radiation treatment for cancer. Radiation can cause scarring and inflammation of lymph nodes or lymph vessels.
- Surgery. In cancer surgery, lymph nodes are often removed to see if the disease has spread. However, this doesn't always result in lymphedema.
- Parasites. In developing countries in the tropics, the most common cause of lymphedema is infection with threadlike worms that clog the lymph nodes.
Less commonly, lymphedema results from inherited conditions in which the lymphatic system doesn't develop properly.
Risk factors
Factors that may increase the risk of developing lymphedema include:
- Older age
- Excess weight or obesity
- Rheumatoid or psoriatic arthritis
Complications
Lymphedema complications may include:
- Skin infections (cellulitis). The trapped fluid provides fertile ground for germs, and the smallest injury to the arm or leg can be an entry point for infection. Affected skin appears swollen and red and is typically painful and warm to the touch. Your doctor may prescribe antibiotics to keep on hand so that you can start taking them immediately.
- Sepsis. Untreated cellulitis can spread into the bloodstream and trigger sepsis — a potentially life-threatening condition that occurs when the body's response to an infection damages its own tissues. Sepsis requires emergency medical treatment.
- Leakage through the skin. With severe swelling, the lymph fluid can drain through small breaks in the skin or cause blistering.
- Skin changes. In some people with very severe lymphedema, the skin of the affected limb can thicken and harden so it resembles the skin of an elephant.
- Cancer. A rare form of soft tissue cancer can result from the most-severe cases of untreated lymphedema.
Nov. 24, 2022