Overview
Vasectomy is a type of birth control that prevents the penis from releasing sperm in fluid called semen during sex. During this minor surgery, a surgeon cuts and seals the tubes that carry sperm.
Vasectomy is a low-risk surgery. Most often, the surgery is done with medicine called a local anesthetic. That means you stay awake and have medicine to numb the surgery area. You'll most likely go home the same day as the surgery. This is called outpatient surgery.
Before getting a vasectomy, you need to be sure that you don't want to start a pregnancy in the future. It's possible to reverse a vasectomy. But the surgery is meant to be a form of birth control that lasts for life.
Vasectomy doesn't protect you from getting or spreading sexually transmitted infections, also called STIs.
Products & Services
Why it's done
Vasectomy is a safe and effective birth control choice. It's meant for people who are certain they don't want to start a pregnancy in the future.
- Vasectomy is nearly 100% effective in preventing pregnancy.
- Vasectomy is an outpatient surgery with a low risk of health concerns called complications or side effects.
- The cost of a vasectomy is far less than the cost of lasting birth control for women called tubal ligation. Vasectomy also is less expensive than the long-term cost of birth control medicines.
- A vasectomy means you won't need to take birth control steps before sex, such as putting on a condom.
Risks
A potential concern with vasectomy is that you might later change your mind about wanting to start a pregnancy. It may be possible to reverse your vasectomy, but there's no guarantee it will work. Reversal surgery is harder to do than a vasectomy. Reversal surgery can be expensive as well. And sometimes, it doesn't work.
The same is true of fertility treatments such as in vitro fertilization, also called IVF. These treatments may be able to help you start a pregnancy after you get a vasectomy. But fertility treatments are expensive, and they don't always work. Before you get a vasectomy, be sure that you don't want to start a pregnancy in the future.
If you have ongoing pain in the testicles or testicular disease, vasectomy likely isn't right for you.
Most people who get a vasectomy don't have side effects that they notice. And serious health troubles due to the surgery are rare.
Side effects right after surgery can include:
- Bleeding or a blood clot inside the pouch of skin that holds the testicles, called the scrotum.
- Blood in the semen.
- Bruising of the scrotum.
- Infection of the surgery site.
- Mild pain or discomfort.
- Swelling.
- A pulling feeling in the scrotum when you move quickly, such as while rising from a chair.
Delayed complications can include:
- Ongoing pain. This can happen for 1% to 2% of people who have a vasectomy.
- Fluid buildup in the testicle. This can cause a dull ache that gets worse when the penis releases semen, called ejaculation.
- Swelling called inflammation that's caused by leaking sperm. This condition is known as a granuloma.
- Pregnancy, in the rare event that a vasectomy doesn't work.
- A sac called a spermatocele that forms in a small, coiled tube on the upper testicle called the epididymis. The epididymis collects and transports sperm.
- A fluid-filled sac called a hydrocele that surrounds a testicle and causes swelling in the scrotum.
The truth about common concerns
Many people worry that a vasectomy could cause serious health problems. But these concerns often aren't grounded in facts. For example, some people worry that a vasectomy might do the following:
- Affect sexual performance. A vasectomy doesn't affect sex drive, erections or masculinity. It only prevents you from starting a pregnancy. Some men have even said they felt more sexual satisfaction after a vasectomy.
- Damage sexual organs. There's very little risk that the testicles, penis or other nearby body parts will be injured during surgery. Very rarely, injury to the blood supply can lead to the loss of a testicle. But that is not likely to happen if your surgeon is skilled.
- Raise cancer risks. There's no proven link between vasectomy and cancer of the testicles or prostate.
- Raise heart disease risk. As with cancer concerns, there doesn't appear to be any link between vasectomy and heart conditions.
- Cause serious pain. You may feel minor pain and pulling or tugging during surgery. But serious pain is rare. Likewise, after surgery you may have some pain. But for most people, the pain is minor and goes away after a few days.
How you prepare
Food and medicines
Your vasectomy surgeon likely will ask you to stop taking certain medicines about a week before surgery. These medicines can include aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). These medicines also can include blood thinners such as warfarin (Jantoven) and heparin. If you take medicine for diabetes, talk with the healthcare professional who prescribes your medicine.
Clothing and personal items
Bring a pair of tightfitting underwear or an athletic supporter to wear after your vasectomy. These can support the scrotum and minimize swelling.
Other steps to take
Shower or bathe on the day of the surgery. Be sure to wash your genital area well. Trim the hair from the front of your scrotum if your surgery teams tells you to do so. Use a disposable razor to trim. Do not use an electric razor or hair removal products.
Arrange for a ride home after your surgery. This helps you prevent movement and pressure on the surgery area caused by driving.
What you can expect
Before
Before doing a vasectomy, your surgeon meets with you to be sure it's the right form of birth control for you.
At this meeting, your surgeon likely will talk with you about:
- How a vasectomy is meant to last for life. It isn't a good choice if there's any chance you might want to start a pregnancy in the future.
- Whether you have children and how your partner feels about the decision, if you're in a relationship.
- Other methods of birth control available to you.
- What vasectomy surgery and recovery involves, and possible complications.
Some family medicine or primary care doctors do vasectomies. But most are done by doctors called urologists who specialize in the male reproductive system.
A vasectomy usually is done with local anesthesia at a doctor's office or surgery center. That means you'll be awake and have medicine to numb the surgery area.
During
Vasectomy
Vasectomy
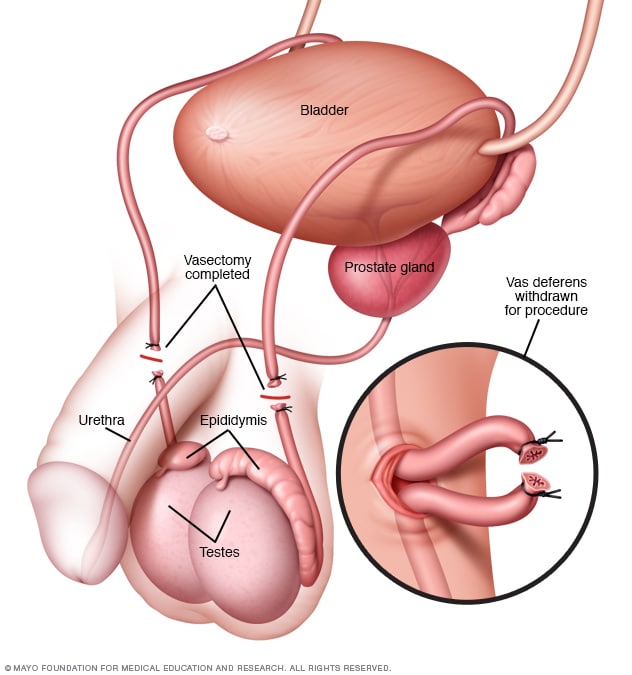
In a vasectomy, the tube that carries sperm from each testicle is cut and sealed. This tube is called the vas deferens.
Vasectomy surgery usually takes about 15 to 20 minutes. To do a vasectomy, your surgeon likely will follow these steps:
- Numb the surgery area by injecting a local anesthetic into the skin of the scrotum with a small needle.
- Make one or two small cuts, also called incisions, in the upper part of the scrotum once the surgery area is numb. Or with the "no-scalpel" technique, make small punctures in the scrotum instead of an incision.
- Locate the tubes called the vas deferens, which carry semen from each testicle.
- Take out part of the vas deferens through the incision or puncture.
- Cut the vas deferens where it has been pulled out of the scrotum.
- Seal the vas deferens by tying it, using heat, placing surgical clips or using a combination of methods. Then your surgeon returns the ends of the vas deferens to the scrotum.
- Close the incision at the surgery area with stitches. If the surgeon made a puncture, the surgeon may close the puncture with glue. Sometimes, the wound may be left to close on its own over time.
After
After a vasectomy, you'll likely have some bruising, swelling and pain. These symptoms usually get better within a few days. A member of your surgery team gives you instructions to help you recover. You'll likely be told to:
- Call right away if you have infection symptoms. These can include blood oozing from the surgery site; a temperature of more than 100.4 degrees Fahrenheit (38 degrees Celsius); a change in skin color; a foul-smelling odor; or pain or swelling that becomes worse.
- Support your scrotum with a bandage and tightfitting underwear for at least three days after your vasectomy.
- Use ice packs to ease discomfort and swelling for the first 2 to 3 days. Cover your scrotum with clothing, a towel or a bed sheet. Then place the ice pack on your covered scrotum.
- Limit activity after surgery. You'll need to rest for 24 hours after surgery. Do not lift objects over 10 pounds or do strenuous activities for at least 48 hours. If you overdo it, that could cause pain or bleeding inside the scrotum. You can probably do light activity after two or three days. Talk with your surgery team about when you can get back to exercise.
- Do not have any sexual activity for 10 days after your vasectomy. If you do ejaculate, you may feel pain or notice blood in your semen. Once you start having sex again, you'll need to use another type of birth control for a time. Use this birth control until your healthcare professional confirms that sperm are no longer present in your semen.
- Take care with bathing. You can shower the day after your vasectomy. But do not directly scrub your scrotum while washing. Also, do not take a bath for one week. After you shower, gently pat the incisions dry with a clean towel.
You also can ease pain with acetaminophen unless your surgery team tells you otherwise.
You still ejaculate semen after a vasectomy. But it takes about 20 ejaculations before you clear out any remaining sperm. A vasectomy blocks new sperm made by the testes from reaching the semen. Instead, the body absorbs the sperm. This is harmless.
Results
A vasectomy doesn't prevent pregnancy right away. Use another form of birth control until your healthcare professional confirms there are no sperm left in your semen. Before you have sex without protection, you'll need to wait a few months or longer. You'll also need to ejaculate about 20 times or more to clear any remaining sperm from your semen.
Most healthcare professionals test semen for sperm about three months after surgery. You'll need to give your healthcare professional semen samples to check. To collect samples, your healthcare professional asks you to masturbate and ejaculate into a container. Or you're asked to use a special condom without lubrication or spermicide to collect semen during sex. Then your semen is checked under a microscope to see whether sperm are present.
Vasectomy is an effective form of birth control. But it won't protect you or your partner from sexually transmitted infections, also called STIs. These include chlamydia and HIV/AIDS. For that reason, keep using other forms of protection such as condoms if you're at risk of getting or spreading STIs.