Risks
Lumpectomy is a surgical procedure that carries a risk of complications and side effects. These can include:
- Bleeding.
- Infection.
- Pain.
- Temporary swelling.
- A scar on the skin of the breast.
- Changes in the shape and appearance of the breast.
How you prepare
To prepare for lumpectomy you'll likely meet with a surgeon. The surgeon may talk about your breast cancer and your treatment options. The surgeon may explain different breast cancer operations and work with you to decide the best one for you. Bring a list of questions. This will help you cover everything you want to know. Make sure you understand the procedure and its risks.
Your healthcare team may give you instructions about things you need to know prior to surgery. The surgery is usually done as an outpatient procedure. This means you typically can go home the same day.
In general, to prepare for your surgery, it's recommended that you:
- Tell your doctor about any medicines, vitamins or supplements you're taking. Some substances could interfere with the surgery.
- Follow your healthcare team's specific instructions. Your healthcare team might have you stop taking certain medicines before the surgery to lower the risk of complications. You may need to stop eating and drinking several hours before surgery.
- Bring someone with you. You will need someone to drive you home after surgery. That person also may need to listen to the healthcare team's instructions about what to do after surgery. The person who comes with you to surgery can help you remember what the care team says.
What you can expect
Locating the area to be removed
Before a lumpectomy, you might have a localization procedure. A localization procedure marks the part of the breast that has the cancer. Your healthcare team often arranges this the day before your lumpectomy surgery. But it could happen several days before your surgery. Sometimes it happens the day of your surgery.
A localization procedure is usually done by a doctor who specializes in imaging tests, called a radiologist. The radiologist uses an imaging test, such as a mammogram or an ultrasound, to locate the cancer in the breast. The radiologist inserts a thin wire, needle or small radioactive seed into the location. The surgeon uses this as a guide to find the precise area that needs to be removed during surgery.
If you have a lump or mass in your breast that can be easily felt through the skin or identified using ultrasound, the localization procedure may not be necessary.
Sentinel lymph node biopsy
Sentinel node biopsy
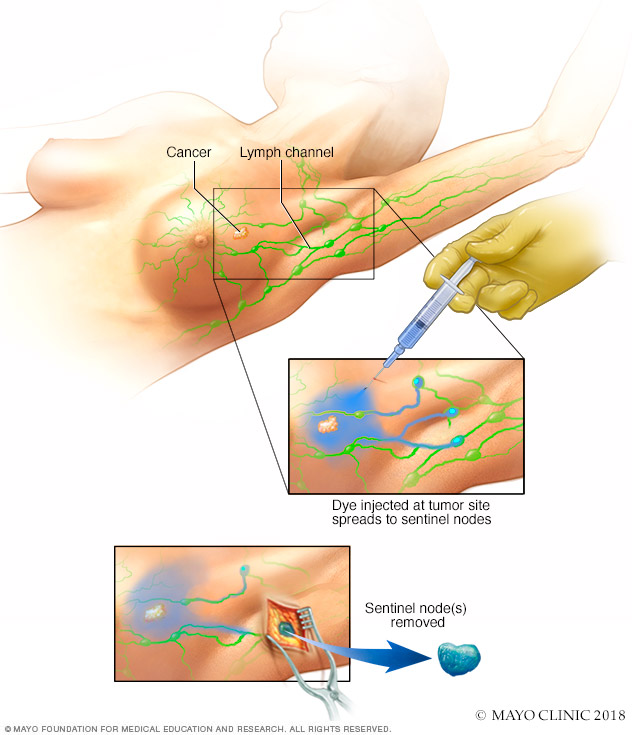
Sentinel node biopsy
Sentinel node biopsy identifies the first few lymph nodes into which a tumor drains. The surgeon uses a harmless dye and a weak radioactive solution to locate the sentinel nodes. The nodes are removed and tested for signs of cancer.
Many people having lumpectomy surgery also have a sentinel lymph node biopsy. Your surgeon may recommend this procedure to remove some lymph nodes near your armpit to see if they contain cancer. When breast cancer spreads, it typically goes to the lymph nodes first. The sentinel lymph nodes are the first lymph nodes where the cancer might spread. A sentinel lymph node biopsy finds and removes these lymph nodes.
To find the sentinel lymph nodes, a healthcare professional injects a radioactive tracer, a blue dye or both into the breast. The tracer and the dye travel to the sentinel nodes. A surgeon makes a cut under your arm to access the lymph nodes. The surgeon removes the lymph nodes that contain tracer and dye.
A healthcare professional examines the lymph nodes under a microscope. If the nodes look free of cancer, the chance of finding cancer in any other lymph nodes is very small. Typically, no other lymph nodes are removed.
If any lymph nodes contain cancer cells, the surgeon might remove more lymph nodes from the armpit to look for cancer. Surgery to remove many lymph nodes from the armpit is called an axillary node dissection.
Sometimes the sentinel lymph nodes don't contain very many cancer cells. In these situations, the surgeon might decide that radiation therapy can treat any cancer cells that remain. An axillary node dissection might not be needed.
Lumpectomy
A lumpectomy is usually performed under general anesthesia. General anesthesia uses medicine to put you into a sleeplike state during the procedure. You aren't aware during the surgery and you won't feel pain. A team of healthcare professionals gives the general anesthetic medicines. The team might include an anesthesiologist and a nurse anesthetist. They watch you closely during the surgery.
Medicine that causes numbness also might be put into the breast. This medicine, called a local anesthetic, helps decrease pain in the breast.
The surgeon makes an incision in the breast. Often the incision is over the cancer or over the area that contains the localization wire or seed. Then the surgeon removes the cancer and some surrounding tissue.
The tissue goes to a lab for testing. In the lab, a doctor who specializes in analyzing tissue, called a pathologist, looks closely at the breast tissue. Sometimes the pathologist recommends removing more of the breast tissue to make sure all the cancer is removed.
The surgeon may place small metallic clips at the site where the cancer was removed. These clips can help with radiation therapy. They show the place where the radiation should go.
The surgeon then uses stitches to close the incisions. These are usually stitches that dissolve over time and do not require removal. Your surgeon also may place thin adhesive strips or use glue on the incision to keep it closed until it heals. Your healthcare team may put you into a surgical bra at the end of your surgery. The bra provides support that helps with swelling. Your healthcare team may ask you to continue wearing it for a while after surgery.
After surgery
Following the procedure, your healthcare team takes you to a recovery area. Your team watches you closely as you come out of your sleeplike state. Most people leave the hospital on the day of surgery. Your healthcare team decides whether it's safe for you to go home.
Expect to have some discomfort after surgery. Your healthcare team might recommend pain medicine to help with the discomfort. Typically this medicine is pain-relieving medicine that you can get without a prescription. Follow your healthcare team's instructions.
Sometimes strong pain medicine is needed. Tell your healthcare team if you have pain. Applying ice to the painful area also might help.
Your healthcare team will likely give you instructions on how to care for yourself at home. The team might go over these instructions with you and the person who helps you get home after surgery. Instructions from your healthcare team might include:
- How to take care of the surgery area.
- What medicines to use for pain.
- When to start taking your usual medicines again.
- Limits on your activity as you recover.
- Warning signs to watch for that might be signs of complications.
- How to contact your healthcare team.
- A list of your next medical appointments.
Results
Ask your healthcare team when you can expect the results of your lumpectomy surgery. Results might be available within a few days. Your healthcare team might call you to talk about the results. Or you might talk about the results at a medical appointment.
The results of lumpectomy surgery are given in a pathology report. A pathology report includes a description of the tissue removed from your breast. It gives the results of lab tests on the tissue.
Sometimes the results of lumpectomy show that you might need more surgery. This can happen if results show that all of the cancer wasn't removed. If this happens, your healthcare team can explain your results and talk about what to expect with another surgery.
After lumpectomy for breast cancer, your healthcare team may have you meet with:
- Your surgical team to answer questions, review your pathology report and check the progress on your healing after surgery.
- A medical oncologist to discuss treatment with medicines for cancer, such as chemotherapy and hormone therapy, which also is called endocrine therapy.
- A radiation oncologist to discuss radiation treatments.
- A counselor or support group to help you cope with having breast cancer.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.