Overview
CT scan slices
CT scan slices
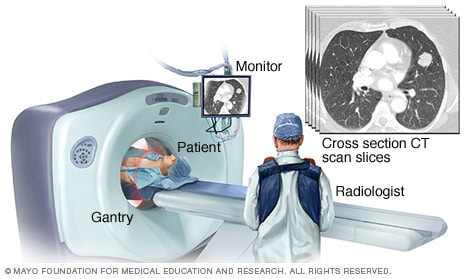
CT scans allow doctors to see cross-sectional images (slices) of your body. This slice shows heart and lung tissue.
Lung cancer screening is a process that's used to detect the presence of lung cancer in otherwise healthy people with a high risk of lung cancer. Lung cancer screening is recommended for older adults who are longtime smokers and who don't have any signs or symptoms of lung cancer.
Doctors use a low-dose computerized tomography (LDCT) scan of the lungs to look for lung cancer. If lung cancer is detected at an early stage, it's more likely to be cured with treatment.
Discuss the benefits and risks of lung cancer screening using LDCT with your doctor. Working together will help you decide whether screening is right for you.
Products & Services
Why it's done
The goal of lung cancer screening is to detect lung cancer at a very early stage — when it's more likely to be cured. By the time lung cancer signs and symptoms develop, the cancer is usually too advanced for curative treatment. Studies show lung cancer screening reduces the risk of dying of lung cancer.
Who should consider screening
Lung cancer screening is usually reserved for people with the greatest risk of lung cancer, including:
- Older adults who are current or former smokers. Lung cancer screening is generally offered to smokers and former smokers who are 50 and older.
-
People who have smoked heavily for many years. You may consider lung cancer screening if you have a history of smoking for 20 pack years or longer. Pack years are calculated by multiplying the number of packs of cigarettes smoked a day and the number of years that you smoked.
For example, a person with 20 pack years of smoking history may have smoked a pack a day for 20 years, two packs a day for 10 years or half of a pack a day for 40 years. Even if your smoking habits changed over the years, your recollection about your smoking history can be used to determine whether lung cancer screening may be beneficial for you.
- People who once smoked heavily but quit. If you were a heavy smoker for a long time and you quit smoking in the last 15 years, you may consider lung cancer screening.
-
People in generally good health. If you have serious health problems, you may be less likely to benefit from lung cancer screening and more likely to experience complications from follow-up tests. For this reason, lung cancer screening is offered to people who are in generally good health.
Screening is generally not recommended for those who have poor lung function or other serious conditions that would make surgery difficult. This might include people who need continuous supplemental oxygen, have experienced unexplained weight loss in the past year, have coughed up blood recently or have had a chest CT scan in the last year.
- People with a history of lung cancer. If you were treated for lung cancer more than five years ago, you may consider lung cancer screening.
- People with other risk factors for lung cancer. People who have other risk factors for lung cancer may include those with chronic obstructive pulmonary disease (COPD), those with a family history of lung cancer and those who have been exposed to asbestos at work.
How long to continue screening
Not all medical groups agree on the age at which you may consider stopping lung cancer screening. In general, continue annual lung cancer screening until you reach a point at which you're unlikely to benefit from screening, such as when you develop other serious health conditions that may make you too frail to undergo lung cancer treatment.
More Information
Risks
Lung cancer screening carries several risks, such as:
- Being exposed to a low level of radiation. The amount of radiation you're exposed to during an LDCT is much less than that of a standard CT scan. It's equal to about half the radiation you're exposed to naturally from the environment in a year.
- Undergoing follow-up tests. If your scan shows a suspicious spot in one of your lungs, you may need to undergo additional scans, which expose you to more radiation, or invasive tests, such as a biopsy, which carry serious risks. If these additional tests show that you don't have lung cancer, you may have been exposed to serious risks that you would have avoided if you didn't undergo screening.
- Finding cancer that's too advanced to cure. Advanced lung cancers, such as those that have spread, may not respond well to treatment, so finding these cancers on a lung cancer screening test might not improve or extend your life.
- Finding cancer that may never hurt you. Some lung cancers grow slowly and may never cause symptoms or harm. It's difficult to know which cancers will never grow to hurt you and which ones must be removed quickly to avoid harm. If you're diagnosed with lung cancer, your doctor will likely recommend treatment. Treatment for cancers that would have remained small and confined the rest of your life may not help you and may be unnecessary.
- Missing cancers. It's possible that lung cancer may be obscured or missed on your lung cancer screening test. In these cases, your results may indicate that you don't have lung cancer when you actually do.
- Finding other health problems. People who smoke for a long time have an increased risk of other health problems, including lung and heart conditions that may be detected on a lung CT scan. If your doctor finds another health problem, you may undergo further testing and, possibly, invasive treatments that wouldn't have been pursued if you hadn't had lung cancer screening.
How you prepare
To prepare for an LDCT scan, you may need to:
- Inform your doctor if you have a respiratory tract infection. If you currently have signs and symptoms of a respiratory tract infection or if you recently recovered from an infection, your doctor may recommend delaying your screening until one month after your signs and symptoms go away. Respiratory infections can cause abnormalities on CT scans that might require additional scans or tests to investigate. These additional tests can be avoided by waiting for the infection to resolve.
-
Remove any metal you're wearing. Metals can interfere with the imaging, so you may be asked to remove any metal that you might be wearing, such as jewelry, glasses, hearing aids and dentures.
Wear clothes that don't have metal buttons or snaps. Don't wear an underwire bra. If your clothing has too much metal, you may be asked to change into a gown.
What you can expect
During lung cancer screening
During an LDCT scan of the lungs, you lie on your back on a long table. You may be given a pillow to make you more comfortable.
The technologist who runs your scan will move to a separate room where he or she can still see you and talk with you.
You'll be asked to lie very still as the table slides through the center of a large machine that creates the images of your lungs. The table passes through the machine initially to determine the starting point for the scan.
When the machine is ready to start the scan, you may be asked to hold your breath briefly to create a clear picture of your lungs. The table will move quickly through the machine as the images are created. The machine may make knocking or clicking noises.
Expect your appointment to last about a half-hour, though the actual scan takes less than a minute.
After lung cancer screening
When your LDCT scan is complete, you can go about your day normally.
The images created during the scan are compiled by a computer and reviewed by a doctor who specializes in diagnosing lung cancer with imaging tests (chest radiologist).
Results
Examples of lung cancer screening results include:
- No abnormalities discovered. If no abnormalities are discovered on your lung cancer screening test, your doctor may recommend you undergo another scan in a year. You may consider continuing annual scans until you and your doctor determine they are unlikely to offer a benefit, such as if you develop other serious health problems.
-
Lung nodules. Lung cancer may appear as a small spot in the lungs. Unfortunately, many other lung conditions look the same, including scars from lung infections and noncancerous (benign) growths. In studies, as many as half the people undergoing lung cancer screening have one or more nodules detected on an LDCT.
Most small nodules don't require immediate action and will be monitored at your next annual lung cancer screening. In some situations, the results may suggest the need for another lung CT scan in a few months to see if the lung nodule grows. Growing nodules are more likely to be cancerous.
A large nodule is more likely to be cancerous. For that reason, you might be referred to a lung specialist (pulmonologist) for additional tests, such as a procedure (biopsy) to remove a piece of a large nodule for laboratory testing, or for additional imaging tests, such as a positron emission tomography (PET) scan.
- Other health problems. Your lung cancer screening test may detect other lung and heart problems that are common in people who have smoked for a long time, such as emphysema and hardening of the arteries in the heart. Discuss these findings with your doctor to determine whether additional tests are needed.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feb. 07, 2024