Nov. 21, 2023
A Mayo Clinic research team discovered that use of intraoperative indocyanine green (ICG) fluorescence angiography is useful for prediction of wound healing complications and for wound prevention in patients undergoing treatment for soft tissue sarcoma. Journal of the American Academy of Orthopaedic Surgeons (AAOS) Global Research & Reviews published the team's findings regarding predictive value of ICG fluorescence in the May 2021 issue. Journal of the American Academy of Orthopaedic Surgeons (JAAOS) then published the researchers' paper about ICG's preventive value in August 2021.
"It basically changed our practice," says Courtney E. Sherman, M.D, an orthopedic oncologist at Mayo Clinic's campus in Florida, who led the research. "This technology gave us eyes beyond human eyes — a window into the blood supply to the patient's skin."
The use of intraoperative ICG fluorescence angiography is not standard across the U.S., she says. Mayo Clinic, however, has the technology necessary for this intraoperative assessment and uses it regularly to benefit the care of patients with soft tissue sarcoma.
 Wound closure
Wound closure
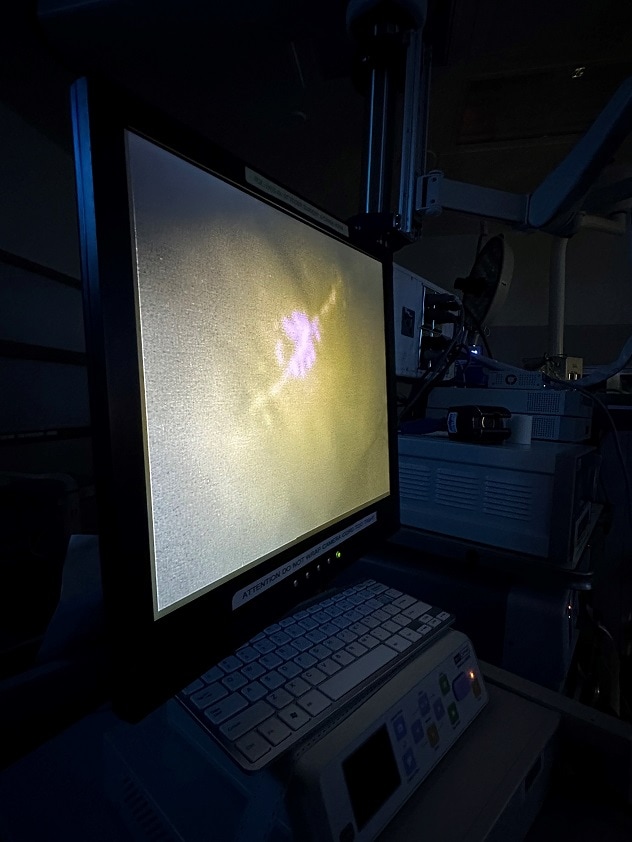
On the monitor, the surgeon intraoperatively views the incision. The white color indicates good blood supply to the skin. If blood supply to the skin were insufficient, the monitor would show a dark spot.
Medical professionals administer ICG fluorescence intravenously for intraoperative assessment of tissue vascularization, according to a 2022 publication by Morales-Conde and colleagues in Spanish Surgery. Receiving information midoperation about what tissue may be at risk of poor healing from the ICG fluorescence allows the surgeon to modify the wound closure. This may involve steps such as altering the flap, using a skin graft or resecting tissue found to have no blood supply.
How wound issues surface for patients with soft tissue sarcoma
To date, wound complications have continued to plague patients with soft tissue sarcoma due to pre-surgical radiation therapy, which affects more than 30% of these patients, indicates the August 2021 JAAOS paper. These complications are challenging to manage for both patients and their surgeons.
Dr. Sherman indicates that typically, patients with soft tissue sarcoma have pre-surgical radiation therapy. Orthopedic oncologists believe that the combination of surgery plus radiation increases the affected limb salvage potential, according to a 2020 article by Wagh and colleagues in Journal of Orthopedic Case Reports. Although surgery and radiation therapy technically could occur in any order, Mayo Clinic orthopedic oncologists have favored administering radiation therapy prior to surgery. The rationale for this order is that the patient can have a lower radiation dose and that pre-surgical radiation has led to fewer long-term scar tissue complications. However, it may increase surgical wound complications.
"It basically changed our practice. This technology gave us eyes beyond human eyes — a window into the blood supply to the patient's skin."
Though modern radiation therapy is significantly more precise than in previous decades, it still may damage the healthy cells alongside cancer cells. Infection may result, or the radiation may destroy the genetic material in healthy cells and cut off blood supply. Over time, the tissue that lacks blood supply necroses, and the patient may require surgery to remove this wounded tissue. Historically, treatment for soft tissue sarcoma with preoperative radiation therapy and surgery for resection carries an infection risk of 38% for all patients. The wound dehiscence risk is 42.3% for all patients who have this treatment protocol, says Dr. Sherman.
"Wound healing issues are a disruption in the patient's treatment," says Dr. Sherman. "Due to wound complications, there has been a lot of 'back to the OR' for patients who have radiation therapy plus surgery for soft tissue sarcoma. It's a big deal if we can keep these patients out of the OR."
The ICG fluorescence studies
In the May 2021 AAOS Global Research & Reviews article by Dr. Sherman and Mayo Clinic colleagues, the investigators demonstrated that intraoperative ICG angiography could predict wound complications postoperatively for patients who had recently received radiation therapy for soft tissue sarcoma. In this prospective 23-patient study, the investigators found that ICG angiography had a sensitivity of 50% and a specificity and positive predictive value of 100%. For patients who had lower extremity resections for soft tissue sarcoma after radiation therapy, ICG angiography had a 70% negative predictive value for wound complications.
Pre-study, the Mayo Clinic investigators suspected that use of the ICG fluorescence dye might predict wound complications but did not have any hypotheses about the intervention value of this dye.
However, they found that ICG fluorescence not only had good predictive value for wound complications for patients who had radiation therapy before surgery but also allowed for specific intervention during the procedure.
For the JAAOS publication in August 2021, the investigators reported on a prospective study conducted between October 2017 and September 2019 in which they collected records for patients undergoing soft tissue sarcoma resections with intraoperative ICG angiography. The investigators compared these patients' experiences to those of historical controls — patients who also had received surgery but before the intraoperative use of ICG angiography. A total of 88 patients were included in the prospective study. Investigators found significantly lower rates of infection (11.8% versus 38%; P = 0.03) and wound dehiscence (11.8% versus 42.3%; P = 0.02) in the ICG angiography cohort compared with the historical controls.
"Using ICG green fluorescence is simple, straightforward and effective, " say Dr. Sherman. "If this is a technology you believe would be helpful with your patients with soft tissue sarcoma, we'd be happy to have you refer them and collaborate with you on their care."
For more information
Wilke BK, et al. A prospective evaluation of intraoperative indocyanine green fluorescence angiography for soft tissue sarcomas. Journal of the American Academy of Orthopaedic Surgeons Global Research & Reviews. 2021;5:e21.00187.
Wilke BK, et al. Intraoperative indocyanine green fluorescence angiography is sensitive for predicting postoperative wound complications in soft-tissue sarcoma surgery. Journal of the American Academy of Orthopaedic Surgeons. 2021;15:433.
Morales-Conde S, et al. Indocyanine green (ICG) fluorescence guide for the use and indications in general surgery: recommendations based on the descriptive review of the literature and the analysis of experience. Spanish Surgery. 2022;100:534.
Wagh Y, et al. Radiation-induced wound infections in operated soft tissue sarcomas: Unbelievable challenge in a series of five cases. Journal of Orthopedic Case Reports. 2020;10:30.
Refer a patient to Mayo Clinic.