April 22, 2023
Mayo Clinic takes a minimally invasive approach to spinal oncology surgery, when appropriate. A multidisciplinary surgical team uses the latest technology to increase longevity and quality of life for patients with primary or metastatic spinal cancer.
"Major open surgery is pretty standard in spinal oncology. But we are performing more of these surgeries minimally invasively or with a 'mini open' approach — opening only the area that needs to be addressed," says Maziyar A. Kalani, M.D., a neurosurgeon at Mayo Clinic in Phoenix/Scottsdale, Arizona.
Spinal metastatic disease is becoming more common, as people with cancer live longer. As many as 30% to 40% of these individuals develop spinal metastases. Although primary tumors of the spinal column are less common, they can be aggressive and cause significant mechanical issues.
"Surgery can have several benefits, in addition to resecting tumors. We are often able to give our patients longer ambulation periods as well as lower rates of incontinence, pneumonia and decubitus ulcers — and therefore longer life expectancy."
Rapid evaluation and expert care
Clear visualization
Clear visualization
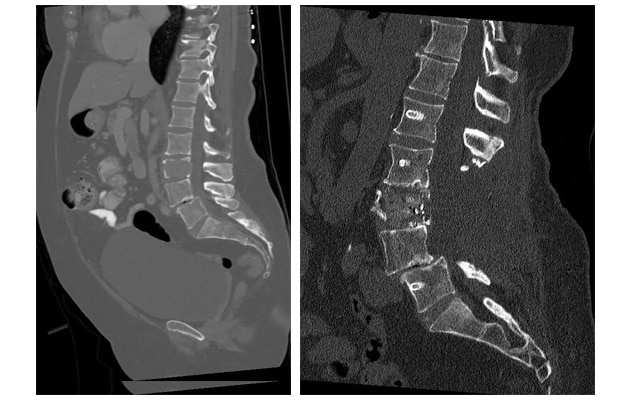
On the left, single-photon emission computerized tomography (SPECT) scan shows a metastatic renal cell lesion. On the right, postoperative SPECT scan indicates successful resection. Imaging with artifact reduction facilitates radiation planning and tumor surveillance.
Mayo Clinic has the technology and expertise needed to perform thorough and timely patient evaluations. Imaging techniques include positron emission tomography (PET) and single-photon emission computerized tomography (SPECT) scans. Biopsies are performed the same day, if needed.
"It's imperative that surgeons be good diagnosticians, especially when patients come to us with an unknown disease pathway. We can then order the evaluations that help ensure they get the right care," Dr. Kalani says.
A multidisciplinary team assesses the imaging and test results and recommends treatment. "Some of these cancers require a multidisciplinary approach," Dr. Kalani says. "Our vascular surgeons are available if an anterior approach is best, and our thoracic surgeons are involved if approaching through the chest makes sense."
The treatment team also might include:
- Specialists in otolaryngology (ENT)/head and neck surgery, for procedures involving complex neck dissections or dissections affecting the brachial plexus.
- Orthopedic surgeons.
- Gynecologic or urologic surgeons.
- Radiation oncologists if intraoperative radiation is needed.
- Plastic surgeons, who can graft bone for complex autografts.
Mayo Clinic uses the latest technology, including carbon-fiber-reinforced polyetheretherketone (CFR-PEEK) surgical implants. In a review published in the March 2023 issue of Skeletal Radiology, Mayo Clinic researchers noted that CFR-PEEK implants offer advantages in terms of biomechanical attributes and postoperative imaging. The implants potentially can have positive impacts on the planning and administration of postoperative radiation therapy.
"Due to the tremendous advances in targeted cancer therapies and surgical strategies, patients are living longer with their cancers," Dr. Kalani says. "We are committed to doing all that we can to preserve quality of life for these patients."
For more information
Long JR, et al. Carbon-fiber-reinforced polyetheretherketone orthopedic implants in musculoskeletal and spinal tumors: Imaging and clinical features. Skeletal Radiology. 2023;52:393.
Refer a patient to Mayo Clinic.