April 11, 2023
Sacral chordoma
Sacral chordoma
Sacral chordoma is a very rare primary malignant tumor affecting the lower sacrum in this case.
With primary malignant tumors of the sacrum, Mayo Clinic orthopedic oncologists must thoroughly and thoughtfully counsel patients regarding the difficult complications inherent to aggressive removal of this type of cancer. Sacrectomy, partial or total, is the gold standard treatment for these tumors. Yet it is a complex, delicate surgery with significant potential morbidity. The No. 1 surgical priority is complete, also called en bloc, removal of the entire cancer to provide the best oncologic outcome. In doing so, the patient may face bowel, bladder, sexual and ambulatory dysfunction, depending on the extent of surgery necessary to remove the cancer.
The most common tumor types affecting the sacrum are metastases from common solid organ malignancies, such as breast or prostate cancer, or hematologic malignancies, such as multiple myeloma. Primary malignant sacral tumors are extraordinarily rare by comparison, with fewer than 1,000 diagnosed annually in the U.S., says Mohammed Karim, M.D., an orthopedic oncologist at Mayo Clinic's campus in Minnesota. Due to these low volumes, primary care physicians or orthopedic surgeons may never encounter a single case in a career, he says. Malignant sacral tumor types include osteosarcoma, malignant peripheral nerve sheath tumors, chondrosarcoma and chordoma.
Diagnostic challenges: Nonspecific findings, rare problem
Primary malignant sacral tumors present significant diagnostic challenges, especially for early diagnosis. Symptoms are vague and difficult for patients or physicians to recognize as a larger condition. Yet, as late diagnosis increases potential morbidity, Dr. Karim says rapidly identifying this malignancy is crucial.
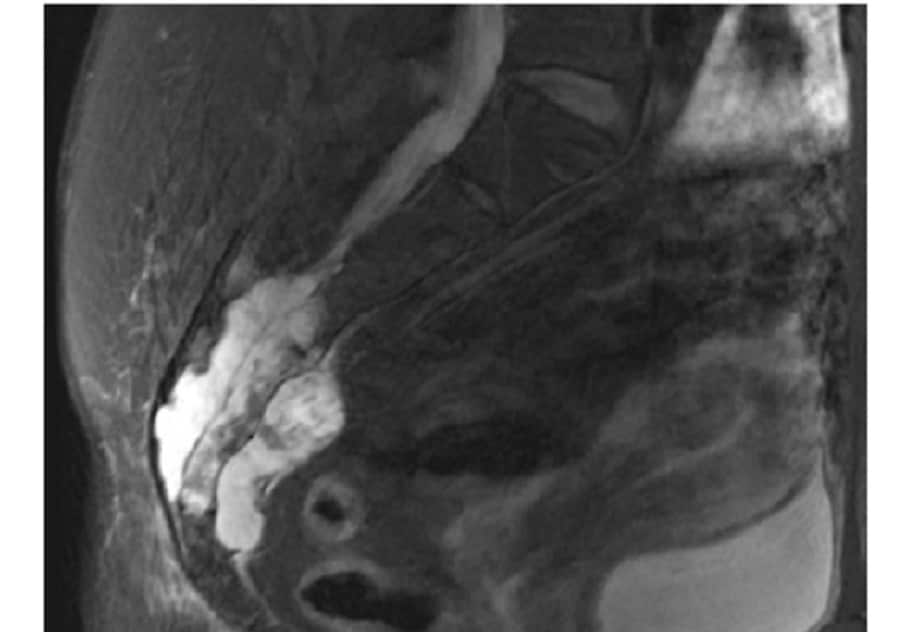
A large chordoma, a primary malignant sacral tumor
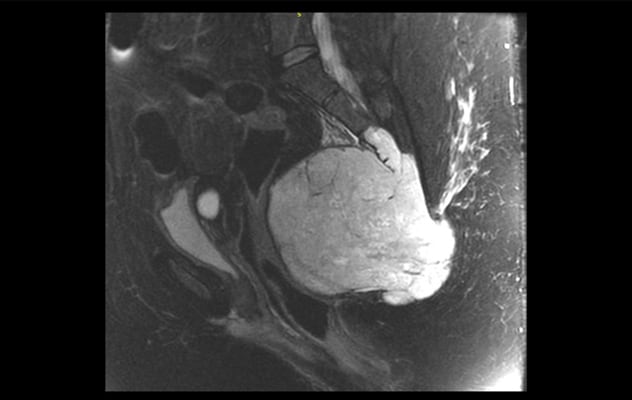
A large chordoma, a primary malignant sacral tumor
Primary malignant sacral tumors can grow to grapefruit or even volleyball size.
Common reasons for patients to see a physician for this type of tumor include unremitting tailbone pain, which is nonspecific, that may or may not be associated with sciatica-like symptoms. Other patients develop an array of symptoms, including tailbone pain, defecation problems such as thinning stool, sexual dysfunction, altered perineal or perigenital sensation, or bladder issues such as urinary retention or incontinence. Tumors can grow to grapefruit or even volleyball size before coming to clinical attention due to the large volume within the pelvis.
As the tumor enlarges, it can entangle the lower sacral nerve roots that control bladder, bowel and sexual functions. The tumor can compress the rectum, resulting in defecation difficulty or altered stool caliber. It can even involve nerves in the pelvis — sciatic, femoral and obturator nerves — that provide motor and sensory function to the lower extremities. Naturally, many of these symptoms are not comfortable for patients to share, even with physicians, as they relate to sexual function and elimination.
"These are all private, personal things to talk about, even to a primary care physician," says Dr. Karim. "This is a barrier to diagnosis."
If patients do present symptoms to a local physician as they arise, it is unlikely that a primary sacral tumor is on the differential since it is such a rare diagnosis. CT or MRI cross-sectional pelvic imaging may detect these tumors. If radiologists identify a sacral mass, physicians should refer the patients urgently to an orthopedic oncology team for additional work-up, including a biopsy to ensure high quality.
Stipulations for effective treatment
Given the rare nature of primary sacral malignancies, multidisciplinary teams at sarcoma centers with knowledge and experience should treat patients with this condition and manage these rare and difficult problems, says Dr. Karim. The following qualities are essential for effective management of these tumors:
Tumor experience
Due to the tumor's rarity, depth of experience with treating it is unusual. Yet, Mayo Clinic is known for addressing this particular malignancy, especially for its proficiency with sacrectomy.
"Mayo Clinic has the reputation and history for treating these malignancies, with considerable experience clinically and a long research history in this area," says Dr. Karim.
Multispecialty team
Treatment for a primary malignant sacral tumor may include chemotherapy, radiotherapy and surgery, depending on factors including tumor histology, cancer staging, anatomic extent of tumor, the patient's medical fitness and the patient's care preferences. Physicians who specialize in each of these disciplines review each case, in addition to radiologists and pathologists who are experts in sarcoma, to provide the patient with options and a consensus recommendation on the best treatment approach.
When orthopedic oncologists undertake surgery, they may perform a full or partial sacrectomy. These operations can be technically difficult and involve multiple stages or days of surgery, with multiple surgical teams involved. These teams may include plastic surgery, colorectal surgery, vascular surgery, urology and others. In addition to the surgical teams, several team members with expertise in anesthesia, ICU, physical medicine and rehabilitation, radiology, pathology, nursing, physical therapy, occupational therapy, nutrition and other areas work to optimize outcomes after these complex surgeries.
Knowledge of proven sacrectomy approaches
Orthopedic oncologists such as those at Mayo Clinic have the background to determine best approaches for patients with distinct malignant sacral tumors. They differentiate these tumors by location in the upper or lower sacrum, addressing lower sacral tumors in one stage with the patient in a prone position for partial sacrectomy. Plastic surgeons close the wound due to the location in a high-risk area near the buttocks.
For upper primary malignant sacral tumors, a multidisciplinary surgical team often operates with the patient in the supine position first to dissect relevant structures and prepare the sacrum for removal through a posterior approach on a second surgical day, usually 24 to 48 hours later. If a colostomy is necessary, a surgeon performs it on the first surgical day. Plastic surgeons will harvest a skin and muscle flap from the abdominal wall on the first surgical day to subsequently inset into the sacrectomy defect on the second surgical day. In some situations, such as a total sacrectomy, the surgeon utilizes spinal hardware — rods and screws along with free vascularized fibular autografts — to reconnect the spine to the pelvis.
Key to optimal malignant sacral tumor resection is en bloc removal — extracting it wholly without debulking, ensuring total removal and likely cure. Any breakage or spillage is a strong risk factor for local recurrence and metastatic spread.
Orthopedic oncologists work with radiation oncologists to decide which patients with malignant sacral tumors may benefit from radiation in addition to surgery. They also decide jointly for which patients radiation, including proton beam therapy, may be an acceptable alternative to surgery.
Skill guiding patients through post-surgical care
Preoperatively, the surgeon determines the extent of sacral resection necessary to remove the entire tumor and explains to the patient the implications of doing so in terms of normal bowel, bladder, sexual and ambulatory functions. With total sacrectomy, Dr. Karim says there is "a 100% chance of bowel, bladder and sexual dysfunction, because you excise all the lower sacral nerves."
Orthopedic oncologists then work alongside physical medicine and rehabilitation physicians before and after surgery to help patients adapt to cancer removal-associated changes. Many patients benefit from spending time at an inpatient rehabilitation unit prior to returning home.
Clinical research generating continuous sacrectomy improvements
Mayo Clinic has pioneered methods for pelvic ring reconstruction after total sacrectomy and spinopelvic resections and published a novel resection classification system. Recent work also has included nerve grafting procedures to help improve bowel and bladder function after sacrectomy.
Referrals for confirmation of diagnosis and sacrectomy
In order to reduce morbidity with malignant primary sacral tumors, Dr. Karim suggests referring patients with newly discovered sacral masses as soon as possible to specialists, such as the orthopedic oncology team at Mayo Clinic in Minnesota, to perform a biopsy and formulate an appropriate treatment plan.
For more information
Refer a patient to Mayo Clinic.