Diagnosis
Lymphoma FAQs
Hematologist Stephen Ansell, M.D., answers the most frequently asked questions about lymphoma.
Well, many times we don't actually know. We do know what exactly happens in the cells. We can see that the cells undergo a genetic change. And as they do that, they may grow quicker than they should, and they may persist and not die off like they should. That causes them to slowly accumulate over time. But exactly what brought about that genetic change, we don't always know.
This is not a disease that's passed down in families, although families can be more susceptible. But we think there are some susceptibility genes that may put you at risk for being more likely to get lymphoma. That does, however, require something else to happen, often in the way of exposures to toxins or viruses or something else.
Well, I think it's important to recognize what the goals of treatment are. Low-grade lymphomas have an advantage in that they can take a very long time to cause any symptoms, and certainly a very long time to put the patient's health at risk. However, we do not have a curative treatment that will fix the cancer right away. So we want to weigh up the potential risks and side effects that come with treatment compared to, clearly, the risks and side effects that come from the cancer. So, if you have a cancer that is very low-grade, growing very slowly, giving you no symptoms, we would hold off on treatment and only initiate it when you truly need it.
Well, important to know that chemotherapy may have two components. Chemotherapy, or chemical drugs that are targeting the cancer, immunotherapy, or antibody treatments that are going after proteins that are on the outside of the cancer or lymphoma cells. The goal of chemotherapy is to kill quickly- growing cells, which is a good thing because lymphoma, many times, those cells are growing quickly. The challenge, however, is there are healthy cells that may also be growing quickly. Immunotherapy, as I mentioned, binds or attacks proteins on the outsides of cells. But some of the lymphoma cells and some of the normal cells have the same proteins. So those cells may be depleted, and your immune system may become a little bit more suppressed as one of the potential side effects of therapy.
Well, I really wish that was true. Unfortunately, that's not exactly correct. There isn't a treatment or exercise program that directly targets or goes after the lymphoma cells. Generally, however, what a healthy balanced diet and a good exercise program is doing is improving your general well-being, improving your immune system function, and allowing you to tolerate the chemotherapy and fight against the cancer to a greater degree. The good news is that many studies have shown that a healthy patient who's in good shape actually has a better outcome when receiving treatment for lymphoma. So that's a strong motivation for you to be healthy by eating well and exercising regularly.
Get as much information as you can. Partner with your physician, your nurse practitioner, your PA and other members of the team and ask questions. The goal moving forward is for you to have the best outcome possible. So that sharing of information between your team and you is critical to your outcome and the best results we could hope for.
Bone marrow exam
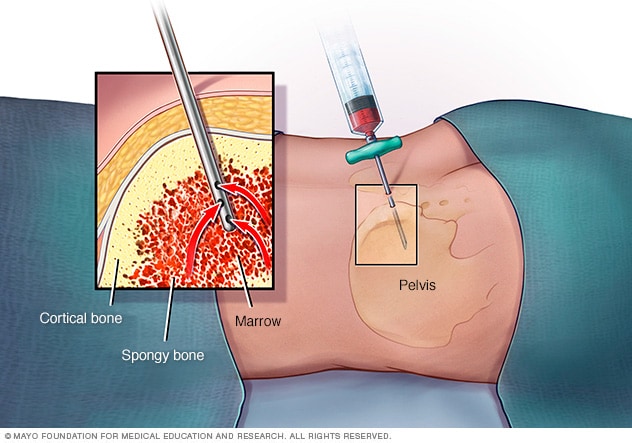
Bone marrow exam
In a bone marrow aspiration, a healthcare professional uses a thin needle to remove a small amount of liquid bone marrow. It is usually taken from a spot in the back of the hipbone, also called the pelvis. A bone marrow biopsy is often done at the same time. This second procedure removes a small piece of bone tissue and the enclosed marrow.
Lymphoma diagnosis often begins with an exam that checks for swollen lymph nodes in the neck, underarm and groin. Other tests include imaging tests and removing some cells for testing. The type of tests used for diagnosis may depend on the lymphoma's location and your symptoms.
Physical Exam
A healthcare professional may start by asking about your symptoms. The health professional also may ask about your health history.
Next, the healthcare professional may feel and press on parts of your body to check for swelling or pain. To find swollen lymph nodes, the health professional may feel your neck, underarm and groin. Be sure to say if you have felt any lumps or pain.
Biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. For lymphoma, the biopsy typically involves removing one or more lymph nodes. The lymph nodes go to a lab for testing to look for cancer cells. Other special tests give more details about the cancer cells. Your healthcare team will use this information to make a treatment plan.
Imaging tests
Your healthcare team may recommend imaging tests to look for signs of lymphoma in other areas of your body. Tests may include CT, MRI and positron emission tomography scans, also called PET scans.
Treatment
Many types of treatments exist for lymphoma. Treatments include radiation, chemotherapy, immunotherapy, targeted therapy and bone marrow transplant, also called stem cell transplant. Sometimes, a combination of treatments is used. The treatment that's best for you will depend on the kind of lymphoma that you have.
Treatment might not need to start right away
Treatment for lymphoma doesn't always need to start right away. Some types of lymphoma grow very slowly. You and your healthcare professional may decide to wait and have treatment if the cancer starts to cause symptoms.
If you don't have treatment, you'll have regular appointments with your healthcare professional to monitor symptoms.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Most chemotherapy medicines are given through a vein. Some come in pill form. Two or more of these medicines together are often used to treat lymphoma.
Immunotherapy
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system to kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells. It can be given for different types of lymphoma.
Targeted therapy
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. Your lymphoma cells might be tested to see if targeted therapy will help you.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy comes from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points in your body.
CAR-T cell therapy
Chimeric antigen receptor (CAR)-T cell therapy, also called CAR-T cell therapy, trains your immune system cells to fight lymphoma. This treatment begins with removing some white blood cells, including T cells, from your blood. The cells are sent to a lab. In the lab, the cells are treated to recognize the lymphoma cells. The cells are then put back into your body. They then can find and destroy the lymphoma cells.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative medicines have been found to treat lymphoma. But integrative medicine may help you cope with the stress of a cancer diagnosis and the side effects of cancer treatment.
Talk to your healthcare professional about your options, such as:
- Acupuncture.
- Art therapy.
- Massage.
- Meditation.
- Music therapy.
- Physical activity.
- Relaxation exercises.
- Yoga.
Coping and support
A lymphoma diagnosis can be overwhelming. With time you'll find ways to cope with the stress and uncertainty that often comes with a lymphoma diagnosis. Until then, you may find that it helps to:
Follow us on Twitter
@MayoCancerCare
Learn about lymphoma
If you'd like to know more about your lymphoma, ask your healthcare professional for the details of your cancer. Ask about the type and your prognosis. Ask for good sources of up-to-date information on your treatment options. Knowing more about your cancer and your options may help you feel more confident when making treatment decisions.
Keep your friends and family close
Your friends and family can be emotional support and provide the practical support you'll need, too, such as helping take care of your house if you're in the hospital.
Find someone to talk with
Find a good listener with whom you can talk about your hopes and fears. This may be a friend or a family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful. Ask your healthcare professional about support groups in your area. You also might contact a cancer organization such as the National Cancer Institute or the Leukemia & Lymphoma Society.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If your healthcare professional suspects that you have lymphoma, that person may refer you to a doctor who specializes in diseases that affect the blood cells. This kind of doctor is called a hematologist.
Appointments can be brief, and there's a lot to discuss. It's a good idea to be prepared. Here's how to help get ready and what to expect:
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if you need to do anything in advance, like restrict your diet.
- Write down any symptoms you're experiencing, even any that may seem unrelated to why you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare professional.
Your time with your healthcare professional is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For lymphoma, some basic questions to ask include:
- Do I have lymphoma?
- What type of lymphoma do I have?
- What stage is my lymphoma?
- Is my lymphoma aggressive or slow growing?
- Will I need more tests?
- Will I need treatment?
- What are my treatment options?
- What are the potential side effects of each treatment?
- How will treatment affect my daily life? Can I continue working?
- How long will treatment last?
- Is there one treatment that you feel is best for me?
- If you had a friend or loved one in my situation, what advice would you give that person?
- Should I see a lymphoma specialist? What will that cost, and will my insurance cover it?
- Do you have brochures or other printed material that I can take with me? What websites do you recommend?
Ask any other questions that come to mind during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you several questions. Being ready to answer them may allow more time to cover other points you want to address. Your healthcare professional may ask:
- When did you first experience symptoms?
- Are your symptoms continuous or occasional?
- How severe are your symptoms?
- What, if anything, helps improve your symptoms?
- What, if anything, worsens your symptoms?
- Has anyone in your family had cancer, including lymphoma?
- Have you or has anyone in your family had immune system conditions?
- Have you or your family been exposed to toxins?