Overview
Blood clot in leg vein

Blood clot in leg vein
A blood clot in a leg vein may cause pain, warmth and tenderness in the affected area.
Thrombophlebitis (throm-boe-fluh-BY-tis) is an inflammatory process that causes a blood clot to form and block one or more veins, usually in the legs. The affected vein might be near the surface of the skin (superficial thrombophlebitis) or deep within a muscle (deep vein thrombosis, or DVT).
Causes of thrombophlebitis include trauma, surgery or prolonged inactivity.
DVT increases the risk of serious health problems. It's usually treated with blood-thinning medications. Superficial thrombophlebitis is sometimes treated with blood-thinning medications, too.
Products & Services
Symptoms
Superficial thrombophlebitis signs and symptoms include:
- Warmth, tenderness and pain in the affected area
- Redness and swelling
Deep vein thrombosis signs and symptoms include:
When a vein close to the surface of the skin is affected, you might see a red, hard cord just under the surface of the skin that's tender to the touch. When a deep vein in the leg is affected, the leg may become swollen, tender and painful.
When to see a doctor
See your doctor right away if you have a red, swollen or tender vein — especially if you have one or more risk factors for thrombophlebitis.
Call 911 or your local emergency number if:
- The vein swelling and pain are severe
- You also have shortness of breath or chest pain, are coughing up blood, or have other symptoms that may indicate a blood clot traveling to your lungs (pulmonary embolism)
Have someone take you to your doctor or emergency room, if possible. It might be difficult for you to drive, and it's helpful to have someone with you to help you remember the information you receive.
Causes
The cause of thrombophlebitis is a blood clot, which can form in your blood as a result of:
- An injury to a vein
- An inherited blood-clotting disorder
- Being immobile for long periods, such as during an injury or a hospital stay
Risk factors
Your risk of thrombophlebitis might increase if you:
- Are inactive for a prolonged period, either because you're confined to bed or you're traveling in a car or plane for a long period
- Have varicose veins, which are a common cause of superficial thrombophlebitis
- Have a pacemaker or have a thin, flexible tube (catheter) in a central vein, for treatment of a medical condition, which may irritate the blood vessel wall and decrease blood flow
- Are pregnant or have just given birth
- Use birth control pills or hormone replacement therapy, which can make your blood more likely to clot
- Have a family history of a blood-clotting disorder or a tendency to form blood clots
- Have had previous episodes of thrombophlebitis
- Have had a stroke
- Are older than 60
- Are overweight or obese
- Have cancer
- Smoke
If you have one or more risk factors, discuss prevention strategies with your doctor before taking long flights or road trips or if you're planning to have elective surgery, recovery from which will require you not to move much.
Complications
Pulmonary embolism
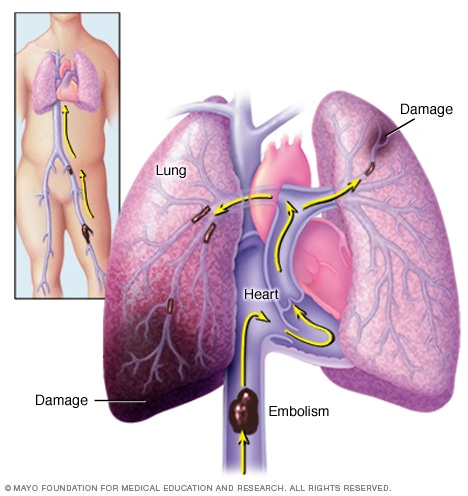
Pulmonary embolism
A pulmonary embolism (PE) occurs when a blood clot gets stuck in an artery in the lung, blocking blood flow to part of the lung. Blood clots most often start in the legs and travel up through the right side of the heart and into the lungs. This is called deep vein thrombosis (DVT).
Complications from superficial thrombophlebitis are rare. However, if you develop DVT, the risk of serious complications increases. Complications might include:
- Blood clot in the lungs (pulmonary embolism). If part of a deep vein clot becomes dislodged, it can travel to your lungs, where it can block an artery (embolism) and become potentially life-threatening.
- Lasting leg pain and swelling (post-phlebetic syndrome). This condition, also known as post-thrombotic syndrome, can develop months or years after you've had DVT. The pain can be disabling.
Prevention
Sitting during a long flight or car ride can cause your ankles and calves to swell and increases your risk of thrombophlebitis. To help prevent a blood clot:
- Take a walk. If you're flying or riding a train or bus, walk up and down the aisle once an hour or so. If you're driving, stop every hour or so and move around.
- Move your legs regularly. Flex your ankles, or carefully press your feet against the floor or footrest in front of you at least 10 times each hour.
- Drink plenty of water or other nonalcoholic fluids to avoid dehydration.
Sept. 04, 2023