Overview
Pulmonary fibrosis
Pulmonary fibrosis
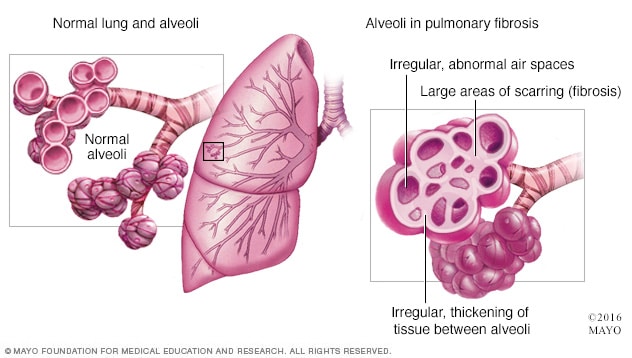
Pulmonary fibrosis is scarred and thickened tissue around and between the air sacs called alveoli in the lungs, as shown on the right. A healthy lung with healthy alveoli is shown on the left.
Pulmonary fibrosis is a lung disease that occurs when lung tissue becomes damaged and scarred. This thickened, stiff tissue makes it harder for the lungs to work properly. Pulmonary fibrosis worsens over time. Some people can stay stable for a long time, but the condition gets worse faster in others. As it gets worse, people become more and more short of breath.
The scarring that happens in pulmonary fibrosis can be caused by many things. Often, doctors and other healthcare professionals cannot pinpoint what's causing the problem. When a cause cannot be found, the condition is called idiopathic pulmonary fibrosis.
Idiopathic pulmonary fibrosis usually occurs in middle-aged and older adults. Sometimes pulmonary fibrosis is diagnosed in children and infants, but this is not common.
The lung damage caused by pulmonary fibrosis cannot be repaired. Medicines and therapies can sometimes help slow down the rate of fibrosis, ease symptoms and improve quality of life. For some people, a lung transplant might be an option.
Products & Services
Symptoms
Symptoms of pulmonary fibrosis may include:
- Shortness of breath.
- Dry cough.
- Extreme tiredness.
- Weight loss that's not intended.
- Aching muscles and joints.
- Widening and rounding of the tips of the fingers or toes, called clubbing.
How fast pulmonary fibrosis worsens over time and how severe the symptoms are can vary greatly from person to person. Some people become ill very quickly with severe disease. Others have moderate symptoms that worsen more slowly, over months or years.
When symptoms suddenly get worse
In people with pulmonary fibrosis, especially idiopathic pulmonary fibrosis, shortness of breath can suddenly get worse over a few weeks or days. This is called an acute exacerbation. It can be life-threatening. The cause of an acute exacerbation may be another condition or an illness, such as a lung infection. But usually the cause is not known.
When to see a doctor
If you have symptoms of pulmonary fibrosis, contact your doctor or other healthcare professional as soon as possible. If your symptoms get worse, especially if they get worse fast, contact your healthcare team right away.
Causes
Pulmonary fibrosis is scarring and thickening of the tissue around and between the air sacs called alveoli in the lungs. These changes make it harder for oxygen to pass into the bloodstream.
Damage to the lungs that results in pulmonary fibrosis may be caused by many different things. Examples include long-term exposure to certain toxins, radiation therapy, some medicines and certain medical conditions. In some cases, the cause of pulmonary fibrosis is not known.
Your work and surroundings
The type of work you do and where you work or live could be the cause or part of the cause for pulmonary fibrosis. Having continuous or repeated contact with toxins or pollutants — substances that harm the quality of water, air or land — can damage your lungs, especially if you do not wear protective gear. Examples include:
- Silica dust.
- Asbestos fibers.
- Hard metal dusts.
- Wood, coal and grain dusts.
- Mold.
- Bird and animal droppings.
Radiation treatments
Some people who receive radiation therapy to the chest, such as for lung or breast cancer, show signs of lung damage months or sometimes years after treatment. How severe the damage is may depend on:
- How much of the lung was exposed to radiation.
- The total amount of radiation given.
- Whether chemotherapy also was used.
- Whether there is underlying lung disease.
Medicines
Many medicines can damage the lungs. Some examples include:
- Chemotherapy. Medicines designed to kill cancer cells, such as methotrexate (Trexall, Otrexup, others), bleomycin and cyclophosphamide (Cytoxan), can damage lung tissue.
- Heart medicines. Some medicines used to treat irregular heartbeats, such as amiodarone (Nexterone, Pacerone), may harm lung tissue.
- Some antibiotics. Antibiotics such as nitrofurantoin (Macrobid, Macrodantin) or ethambutol (Myambutol) can cause lung damage.
- Anti-inflammatory medicines. Certain anti-inflammatory medicines such as rituximab (Rituxan) or sulfasalazine (Azulfidine) can cause lung damage.
Medical conditions
Lung damage can also result from a number of conditions, including:
- Dermatomyositis, an inflammatory disease marked by muscle weakness and a skin rash.
- Lupus, a disease that occurs when the body's immune system attacks its own tissues and organs.
- Mixed connective tissue disease, which has a mix of symptoms of different disorders, such as lupus, scleroderma and polymyositis.
- Pneumonia, an infection that inflames the air sacs in one or both lungs.
- Polymyositis, an inflammatory disease that causes muscle weakness on both sides of the body.
- Rheumatoid arthritis, an inflammatory disease that affects joints and other body systems.
- Sarcoidosis, an inflammatory disease that most often affects the lungs and lymph nodes.
- Scleroderma, a group of rare diseases that involve hardening and tightening of the skin as well as problems inside the body.
Idiopathic pulmonary fibrosis
Many substances and conditions can lead to pulmonary fibrosis. Even so, in many people, the cause is never found. But risk factors such as smoking or exposure to air pollution could be related to the condition, even if the cause cannot be confirmed. Pulmonary fibrosis with no known cause is called idiopathic pulmonary fibrosis.
Many people with idiopathic pulmonary fibrosis also may have gastroesophageal reflux disease, also called GERD. This condition occurs when acid from the stomach flows back into the esophagus. GERD may be a risk factor for idiopathic pulmonary fibrosis or cause the condition to worsen faster. But more studies are needed.
Risk factors
Pulmonary fibrosis has been found in children and infants, but this is not common. Idiopathic pulmonary fibrosis is much more likely to affect middle-aged and older adults. Other types of pulmonary fibrosis, such as that caused by connective tissue disease, can occur in younger people.
Factors that can raise your risk of pulmonary fibrosis include:
- Smoking. If you smoke now or used to smoke, you're at a higher risk of pulmonary fibrosis than people who never smoked. People with emphysema are at higher risk, too.
- Certain types of work. You have a higher risk of developing pulmonary fibrosis if you work in mining, farming or construction. The risk also is higher if you have continuous or repeated contact with pollutants known to damage the lungs.
- Cancer treatments. Having radiation treatments to your chest or using certain chemotherapy medicines can raise your risk of pulmonary fibrosis.
- Genetics. Some types of pulmonary fibrosis run in families, so genes may play a role.
Complications
Complications of pulmonary fibrosis may include:
- High blood pressure in the lungs. Called pulmonary hypertension, this type of high blood pressure affects the arteries in the lungs. These are the pulmonary arteries. Stiff and thick arteries may slow down or block blood flow through the lungs. This raises the pressure inside the pulmonary arteries and the lower right heart chamber, called the right ventricle.
- Right-sided heart failure. This serious condition occurs when your heart's right chamber has to pump harder than usual to move blood through partly blocked pulmonary arteries.
- Respiratory failure. This is often the last stage of long-term lung disease. It occurs when blood oxygen levels fall dangerously low.
- Lung cancer. Long-standing pulmonary fibrosis increases your risk of developing lung cancer.
- Other lung problems. As pulmonary fibrosis gets worse over time, it may lead to serious problems such as blood clots in the lungs, a collapsed lung or lung infections.
Feb. 15, 2024