Overview
Diabetic nephropathy is a serious complication of type 1 diabetes and type 2 diabetes. It's also called diabetic kidney disease. In the United States, about 1 in 3 people living with diabetes have diabetic nephropathy.
Diabetic nephropathy affects the kidneys' usual work of removing waste products and extra fluid from the body. The best way to prevent or delay diabetic nephropathy is by living a healthy lifestyle and keeping diabetes and high blood pressure managed.
Over years, diabetic nephropathy slowly damages the kidneys' filtering system. Early treatment may prevent this condition or slow it and lower the chance of complications.
Diabetic kidney disease can lead to kidney failure. This also is called end-stage kidney disease. Kidney failure is a life-threatening condition. Treatment options for kidney failure are dialysis or a kidney transplant.
One of the important jobs of the kidneys is to clean the blood. As blood moves through the body, it picks up extra fluid, chemicals and waste. The kidneys separate this material from the blood. It's carried out of the body in urine. If the kidneys are unable to do this and the condition is untreated, serious health problems result, with eventual loss of life.
Products & Services
Symptoms
In the early stages of diabetic nephropathy, there might not be symptoms. In later stages, symptoms may include:
- High blood pressure that gets harder to control.
- Swelling of feet, ankles, hands or eyes.
- Foamy urine.
- Confusion or difficulty thinking.
- Shortness of breath.
- Loss of appetite.
- Nausea and vomiting.
- Itching.
- Tiredness and weakness.
When to see a doctor
Make an appointment with your health care professional if you have symptoms of kidney disease. If you have diabetes, visit your health care professional yearly or as often as you're told for tests that measure how well your kidneys are working.
Causes
Diabetic nephropathy happens when diabetes damages blood vessels and other cells in the kidneys.
How the kidneys work
Healthy kidney vs. diseased kidney
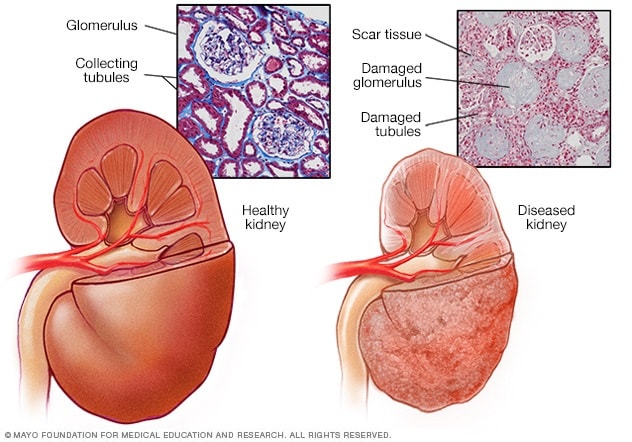
Healthy kidney vs. diseased kidney
A typical kidney has about 1 million filtering units. Each unit, called a glomerulus, joins a tubule. The tubule collects urine. Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring.
Kidney cross section
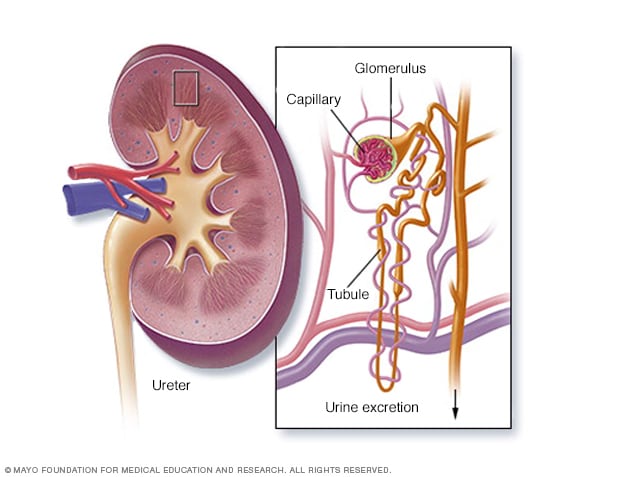
Kidney cross section
The kidneys remove waste and extra fluid from the blood through filtering units called nephrons. Each nephron contains a filter, called a glomerulus. Each filter has tiny blood vessels called capillaries. When blood flows into a glomerulus, tiny bits, called molecules, of water, minerals and nutrients, and wastes pass through the capillary walls. Large molecules, such as proteins and red blood cells, do not. The part that's filtered then passes into another part of the nephron called the tubule. The water, nutrients and minerals the body needs are sent back to the bloodstream. The extra water and waste become urine that flows to the bladder.
The kidneys have millions of tiny blood vessel clusters called glomeruli. Glomeruli filter waste from the blood. Damage to these blood vessels can lead to diabetic nephropathy. The damage can keep the kidneys from working as they should and lead to kidney failure.
Diabetic nephropathy causes
Diabetic nephropathy is a common complication of type 1 and type 2 diabetes.
Over time, diabetes that isn't well controlled can damage blood vessels in the kidneys that filter waste from the blood. This can lead to kidney damage and cause high blood pressure.
High blood pressure can cause more kidney damage by raising the pressure in the filtering system of the kidneys.
Risk factors
If you have diabetes, the following can raise your risk of diabetic nephropathy:
- Uncontrolled high blood sugar, also called hyperglycemia.
- Uncontrolled high blood pressure, also called hypertension.
- Smoking.
- High blood cholesterol.
- Obesity.
- A family history of diabetes and kidney disease.
Complications
Complications of diabetic nephropathy can come on slowly over months or years. They may include:
- Body fluid buildup. This could lead to swelling in the arms and legs, high blood pressure, or fluid in the lungs, called pulmonary edema.
- A rise in the levels of the mineral potassium in the blood, called hyperkalemia.
- Heart and blood vessel disease, also called cardiovascular disease. This could lead to a stroke.
- Fewer red blood cells to carry oxygen. This condition also is called anemia.
- Pregnancy complications that carry risks for the pregnant person and the growing fetus.
- Damage to the kidneys that can't be fixed. This is called end-stage kidney disease. Treatment is either dialysis or a kidney transplant.
Prevention
To lower your risk of developing diabetic nephropathy:
- See your health care team regularly to manage diabetes. Keep appointments to check on how well you are managing your diabetes and to check for diabetic nephropathy and other complications. Your appointments might be yearly or more often.
- Treat your diabetes. With good treatment of diabetes, you can keep your blood sugar levels in the target range as much as possible. This may prevent or slow diabetic nephropathy.
- Manage high blood pressure or other medical conditions. If you have high blood pressure or other conditions that raise your risk of kidney disease, work with your health care professional to control them.
- Take medicines you get without a prescription only as directed. Read the labels on the pain relievers you take. This might include aspirin and nonsteroidal anti-inflammatory drugs, such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others). For people with diabetic nephropathy, these types of pain relievers can lead to kidney damage.
- Stay at a healthy weight. If you're at a healthy weight, work to stay that way by being physically active most days of the week. If you need to lose weight, talk with a member of your health care team about the best way for you to lose weight.
- Don't smoke. Cigarette smoking can damage kidneys or make kidney damage worse. If you're a smoker, talk to a member of your health care team about ways to quit. Support groups, counseling and some medicines might help.
Oct. 24, 2023