Overview
Pancreatitis caused by gallstones
Pancreatitis caused by gallstones
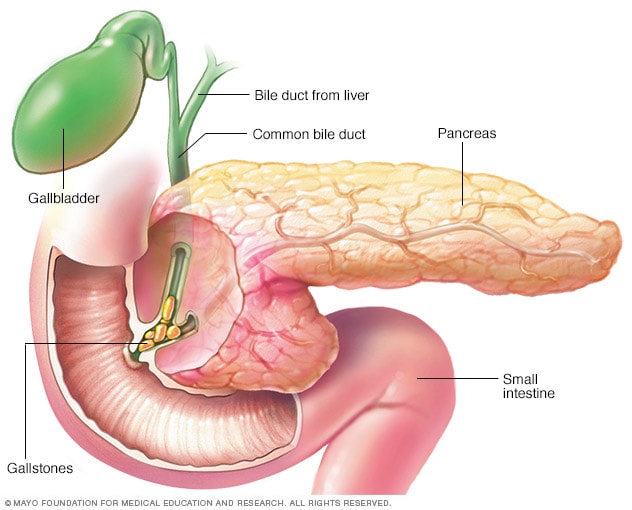
Gallstones are a common cause of pancreatitis. Gallstones, produced in the gallbladder, can slip out of the gallbladder and block the bile duct, stopping pancreatic enzymes from traveling to the small intestine and forcing them back into the pancreas. The enzymes then begin to irritate the cells of the pancreas, causing the inflammation associated with pancreatitis.
Pancreatitis is inflammation of the pancreas. Inflammation is immune system activity that can cause swelling, pain, and changes in how an organ or tissues work.
The pancreas is a long, flat gland that's tucked behind the stomach. The pancreas helps the body digest food and regulates blood sugars.
Pancreatitis can be an acute condition. This means it appears suddenly and generally lasts a short time. Chronic pancreatitis is a long-term condition. The damage to the pancreas can get worse over time.
Acute pancreatitis may improve on its own. More-serious disease requires treatment in a hospital and can cause life-threatening complications.
Products & Services
Symptoms
Symptoms of pancreatitis may vary. Acute pancreatitis symptoms may include:
- Pain in the upper belly.
- Pain in the upper belly that radiates to the back.
- Tenderness when touching the belly.
- Fever.
- Rapid pulse.
- Upset stomach.
- Vomiting.
Chronic pancreatitis signs and symptoms include:
- Pain in the upper belly.
- Belly pain that feels worse after eating.
- Losing weight without trying.
- Oily, smelly stools.
Some people with chronic pancreatitis only develop symptoms after they get complications of the disease.
When to see a doctor
Make an appointment with your doctor if you have sudden belly pain or belly pain that doesn't improve. Seek immediate medical help if your pain is so severe that you can't sit still or find a position that makes you more comfortable.
Causes
The pancreas has two major roles. It produces insulin, which helps the body manage and use sugars.
The pancreas also produces dietary juices, called enzymes, that help with digestion. The pancreas makes and stores "turned off" versions of the enzymes. After the pancreas sends the enzymes into the small intestine, they are "turned on" and break down proteins in the small intestine.
If the enzymes are turned on too soon, they can start acting like digestive juices inside the pancreas. The action can irritate, damage or destroy cells. This problem, in turn, leads to immune system responses that cause swelling and other events that affect how the pancreas works.
Several conditions can lead to acute pancreatitis, including:
- Blockage in the bile duct caused by gallstones.
- Heavy alcohol use.
- Certain medicines.
- High triglyceride levels in the blood.
- High calcium levels in the blood.
- Pancreas cancer.
- Injuries from trauma or surgery.
Conditions that can lead to chronic pancreatitis include:
- Damage from repeated acute pancreatitis.
- Heavy alcohol use.
- Inherited genes linked to pancreatitis.
- High triglyceride levels in the blood.
- High calcium levels in the blood.
Sometimes, a cause for pancreatitis is never found. This is known as idiopathic pancreatitis.
Risk factors
Factors that increase your risk of pancreatitis include:
- Excessive alcohol use. Research shows that having four or five drinks a day increases the risk of pancreatitis.
- Cigarette smoking. Compared with nonsmokers, smokers are on average three times more likely to develop chronic pancreatitis. Quitting smoking can decrease the risk.
- Obesity. People with a body mass index of 30 or higher are at increased risk of pancreatitis.
- Diabetes. Having diabetes increases the risk of pancreatitis.
- Family history of pancreatitis. A number of genes have been linked to chronic pancreatitis. A family history of the disease is linked to an increased risk, especially when combined with other risk factors.
Complications
Pancreatitis can cause serious complications, including:
- Kidney failure. Acute pancreatitis may result in the kidneys not filtering waste from the blood. Artificial filtering, called dialysis, may be needed for short-term or long-term treatment.
- Breathing problems. Acute pancreatitis can cause changes in how the lungs work, causing the level of oxygen in the blood to fall to dangerously low levels.
- Infection. Acute pancreatitis can make the pancreas vulnerable to infections. Pancreatic infections are serious and require intensive treatment, such as surgery or other procedures to remove the infected tissue.
- Pseudocyst. Acute and chronic pancreatitis can cause fluid and debris to collect in a "pocket" in the pancreas, called a pseudocyst. A large pseudocyst that ruptures can cause complications such as internal bleeding and infection.
- Malnutrition. With both acute and chronic pancreatitis, the pancreas may not produce enough enzymes for the digestive system. This can lead to malnutrition, diarrhea and weight loss.
- Diabetes. Diabetes can develop when chronic pancreatitis damages cells that produce insulin.
- Pancreatic cancer. Long-standing inflammation in the pancreas is a risk factor for cancer of the pancreas.
Sept. 23, 2023