Diagnosis
A diagnosis of uterine prolapse often occurs during a pelvic exam. During the pelvic exam your health care provider may have you:
- Bear down as if having a bowel movement. This can help your provider assess how far the uterus has slipped into the vagina.
- Tighten your pelvic muscles as if you're stopping a stream of urine. This test checks the strength of pelvic muscles.
You also might fill out a questionnaire. This helps your provider assess how uterine prolapse affects your life. This information helps guide treatment decisions.
If you have severe urinary incontinence, you might have tests to measure how well your bladder works. This is called urodynamic testing.
More Information
Treatment
Types of pessaries
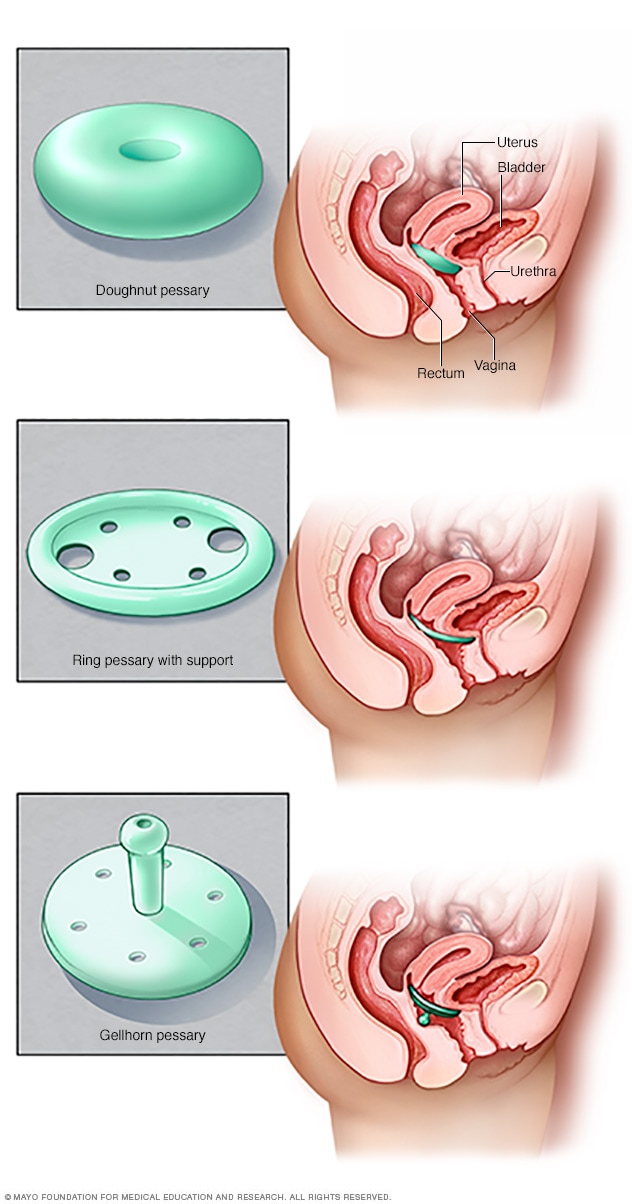
Types of pessaries
Pessaries come in many shapes and sizes. The device fits into the vagina and provides support to vaginal tissues displaced by pelvic organ prolapse. A health care provider can fit a pessary and help provide information about which type would work best.
If you have uterine prolapse and it doesn't bother you, treatment may not be needed. You might choose to wait and see what happens. But when prolapse symptoms bother you, your provider may suggest:
- Self-care measures. Self-care measures might provide relief from symptoms or help prevent the prolapse from getting worse. Self-care measures include performing exercises to strengthen pelvic muscles. These are called Kegel exercises. You might also benefit from losing weight and treating constipation.
- A pessary. A vaginal pessary is a silicone device inserted into the vagina. It helps prop up bulging tissues. A pessary must be removed regularly for cleaning.
Surgery
Surgery may be needed to repair uterine prolapse. Minimally invasive surgery, called laparoscopic surgery, or vaginal surgery might be an option.
If you only have a uterine prolapse, surgery may involve:
- Taking out the uterus. This is called a hysterectomy. Hysterectomy may be recommended for uterine prolapse.
- A procedure that keeps the uterus in place. This is called a uterus-sparing procedure. These surgeries are for people who might want to have another pregnancy. There is less information on how effective these types of surgeries are. More study is needed.
But if you have prolapse of other pelvic organs along with uterine prolapse, surgery may be a bit more involved. Along with a hysterectomy to take out the uterus, your surgeon may also:
- Use stitches to fix weak pelvic floor structures. This can be done in a way that keeps the depth and width of the vagina intact for sexual function.
- Close the opening of the vagina. This procedure is called a colpocleisis. It may allow for an easier recovery from surgery. This surgery is only an option for those who no longer want to use the vaginal canal for sexual activity.
- Place a piece of mesh to support vaginal tissues. In this procedure, vaginal tissues are suspended from the tail bone using a synthetic mesh material.
All surgeries have risks. Risks of surgery for uterine prolapse include:
- Heavy bleeding
- Blood clots in the legs or lungs
- Infection
- A bad reaction to anesthesia
- Injury to other organs including the bladder, ureters or bowel
- Prolapse happens again
- Urinary incontinence
Talk with your health care provider about all your treatment options to be sure you understand the risks and benefits of each.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Depending on how severe uterine prolapse is, self-care measures might provide relief from symptoms. You might try to:
- Strengthen the muscles that support pelvic structures
- Eat high-fiber foods and drink lots of fluids to avoid constipation
- Avoid bearing down during bowel movements
- Avoid heavy lifting
- Control coughing
- Lose weight if you're overweight
- Quit smoking
Kegel exercises
Kegel exercises can strengthen pelvic floor muscles. A strong pelvic floor provides better support for pelvic organs. This might relieve symptoms that can happen with uterine prolapse.
To do these exercises:
- Tighten pelvic floor muscles as though trying to prevent passing gas.
- Hold the contraction for five seconds, and then relax for five seconds. If this is too difficult, start by holding for two seconds and relaxing for three seconds.
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions every day.
Kegel exercises might be most successful when a physical therapist teaches them and reinforces the exercises with biofeedback. Biofeedback uses monitoring devices that help ensure proper tightening of the muscles for long enough to work well.
Once you learn how to do them properly, you can do Kegel exercises discreetly just about anytime, whether sitting at a desk or relaxing on the couch.
Preparing for your appointment
For uterine prolapse, you may see a doctor who specializes in conditions affecting the female reproductive system. This type of doctor is called a gynecologist. Or you may see a doctor who specializes in pelvic floor problems and reconstructive surgery. This type of doctor is called a urogynecologist.
Here's some information to help you get ready for your appointment.
What you can do
Make a list of:
- Your symptoms and when they began
- All medicine, vitamins and supplements you take, including the doses
- Key personal and medical information, including other conditions, recent life changes and stressors
- Questions to ask your health care provider
For uterine prolapse, some basic questions to ask include:
- What can I do at home to ease my symptoms?
- What are the chances that the prolapse will worsen if I don't do anything?
- What treatment approach do you recommend?
- How likely is it that uterine prolapse will happen again if I have surgery to treat it?
- What are the risks of surgery?
Don't hesitate to ask other questions you have.
What to expect from your doctor
Your provider is likely to ask you questions, including:
- Have your symptoms gotten worse?
- Do you have pelvic pain?
- Do you ever leak urine?
- Have you had a severe or ongoing cough?
- Do you do heavy lifting in your job or daily activities?
- Do you strain during bowel movements?
- Has anyone in your family had uterine prolapse or other pelvic problems?
- How many children have you given birth to? Were your deliveries vaginal?
- Do you plan to have children in the future?
Sept. 08, 2022