Overview
Male hypogonadism is a condition in which the body doesn't produce enough of the hormone that plays a key role in masculine growth and development during puberty (testosterone) or enough sperm or both.
You can be born with male hypogonadism, or it can develop later in life, often from injury or infection. The effects — and what you can do about them — depend on the cause and at what point in your life male hypogonadism occurs. Some types of male hypogonadism can be treated with testosterone replacement therapy.
Symptoms
Hypogonadism can begin during fetal development, before puberty or during adulthood. Signs and symptoms depend on when the condition develops.

Male reproductive system
The male reproductive system makes, stores and moves sperm. Testicles produce sperm. Fluid from the seminal vesicles and prostate gland combine with sperm to make semen. The penis ejaculates semen during sexual intercourse.
Fetal development
If the body doesn't produce enough testosterone during fetal development, the result may be impaired growth of the external sex organs. Depending on when hypogonadism develops and how much testosterone is present, a child who is genetically male may be born with:
- Female genitals
- Genitals that are neither clearly male nor clearly female (ambiguous genitals)
- Underdeveloped male genitals
Puberty
Male hypogonadism can delay puberty or cause incomplete or lack of normal development. It can hamper:
- Development of muscle mass
- Voice deepening
- Growth of body and facial hair
- Growth of the penis and testicles
And it can cause:
- Excessive growth of the arms and legs in relation to the trunk of the body
- Development of breast tissue (gynecomastia)
Adulthood
In adult males, hypogonadism can alter certain masculine physical characteristics and impair normal reproductive function. Early signs and symptoms might include:
- Decreased sex drive
- Decreased energy
- Depression
Over time, men with hypogonadism can develop:
- Erectile dysfunction
- Infertility
- Decrease in hair growth on the face and body
- Decrease in muscle mass
- Development of breast tissue (gynecomastia)
- Loss of bone mass (osteoporosis)
Severe hypogonadism can also cause mental and emotional changes. As testosterone decreases, some men have symptoms similar to those of menopause in women. These can include:
- Difficulty concentrating
- Hot flashes
When to seek help
See your health care provider if you have symptoms of male hypogonadism. Finding the cause of hypogonadism is an important first step to getting appropriate treatment.
Causes
Male hypogonadism means the testicles don't produce enough of the male sex hormone testosterone. There are two basic types of hypogonadism:
- Primary. This type of hypogonadism — also known as primary testicular failure — originates from a problem in the testicles.
- Secondary. This type of hypogonadism indicates a problem in the hypothalamus or the pituitary gland — parts of the brain that signal the testicles to produce testosterone. The hypothalamus produces gonadotropin-releasing hormone, which signals the pituitary gland to make follicle-stimulating hormone (follicle-stimulating hormone (FSH)) and luteinizing hormone (luteinizing hormone (LH)). Luteinizing hormone then signals the testes to produce testosterone.
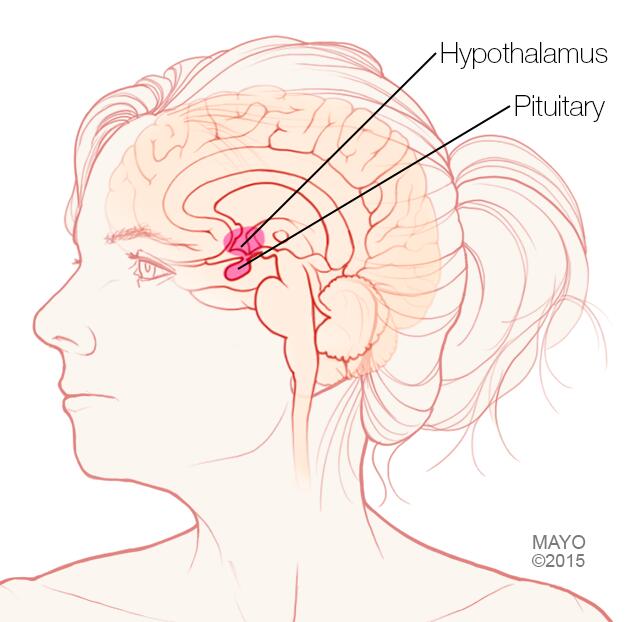
Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus are located within the brain and control hormone production.
Either type of hypogonadism can be caused by an inherited (congenital) trait or something that happens later in life (acquired), such as an injury or an infection. At times, primary and secondary hypogonadism occur together.
Primary hypogonadism
Common causes of primary hypogonadism include:
-
Klinefelter syndrome. This condition results from a congenital abnormality of the sex chromosomes, X and Y. A male normally has one X and one Y chromosome. In Klinefelter syndrome, two or more X chromosomes are present in addition to one Y chromosome.
The Y chromosome contains the genetic material that determines the sex of a child and related development. The extra X chromosome that occurs in Klinefelter syndrome causes abnormal development of the testicles, which in turn results in underproduction of testosterone.
-
Undescended testicles. Before birth, the testicles develop inside the abdomen and normally move down into their permanent place in the scrotum. Sometimes one or both of the testicles aren't descended at birth.
This condition often corrects itself within the first few years of life without treatment. If not corrected in early childhood, it can lead to malfunction of the testicles and reduced production of testosterone.
- Mumps orchitis. A mumps infection involving the testicles that occurs during adolescence or adulthood can damage the testicles, affecting the function of the testicles and testosterone production.
- Hemochromatosis. Too much iron in the blood can cause testicular failure or pituitary gland dysfunction, affecting testosterone production.
- Injury to the testicles. Because they're outside the abdomen, the testicles are prone to injury. Damage to both testicles can cause hypogonadism. Damage to one testicle might not impair total testosterone production.
-
Cancer treatment. Chemotherapy or radiation therapy for the treatment of cancer can interfere with testosterone and sperm production. The effects of both treatments often are temporary, but permanent infertility may occur.
Although many men regain their fertility within a few months after treatment, preserving sperm before starting cancer therapy is an option for men.
Secondary hypogonadism
In secondary hypogonadism, the testicles are normal but don't function properly due to a problem with the pituitary or hypothalamus. A number of conditions can cause secondary hypogonadism, including:
- Kallmann's syndrome. This is an abnormal development of the area of the brain that controls the secretion of pituitary hormones (hypothalamus). This abnormality can also affect the ability to smell (anosmia) and cause red-green color blindness.
-
Pituitary disorders. An abnormality in the pituitary gland can impair the release of hormones from the pituitary gland to the testicles, affecting normal testosterone production. A pituitary tumor or other type of brain tumor located near the pituitary gland may cause testosterone or other hormone deficiencies.
Also, treatment for a brain tumor, such as surgery or radiation therapy, can affect the pituitary gland and cause hypogonadism.
- Inflammatory disease. Certain inflammatory diseases, such as sarcoidosis, histiocytosis and tuberculosis, involve the hypothalamus and pituitary gland and can affect testosterone production.
- HIV/AIDS. HIV/AIDS can cause low levels of testosterone by affecting the hypothalamus, the pituitary and the testes.
- Medications. The use of certain drugs, such as opiate pain medications and some hormones, can affect testosterone production.
- Obesity. Being significantly overweight at any age might be linked to hypogonadism.
- Aging. As men age, there's a slow, progressive decrease in testosterone production. The rate varies greatly.
Risk factors
Risk factors for hypogonadism include:
- HIV/AIDS
- Previous chemotherapy or radiation therapy
- Aging
- Obesity
- Malnutrition
Hypogonadism can be inherited. If any of these risk factors are in your family health history, tell your doctor.
Complications
The complications of untreated hypogonadism differ depending on when it develops — during fetal development, puberty or adulthood.
Complications might include:
- Abnormal genitalia
- Enlarged male breasts (gynecomastia)
- Infertility
- Erectile dysfunction
- Osteoporosis
- Poor self-image