Diagnosis
To diagnose a heart arrhythmia, a healthcare professional examines you and asks about your medical history and symptoms.
You may have tests to check your heart and to look for health conditions that can cause an irregular heartbeat.
Tests
Tests to diagnose a heart arrhythmia may include:
- Electrocardiogram (ECG or EKG). This quick test measures the electrical activity of the heart. It can show how fast or how slow the heart is beating. Sticky patches called sensors are attached to the chest and sometimes to the arms or legs. Wires connect the patches to a computer, which displays or prints results.
- Holter monitor. This portable ECG device can be worn for a day or more to record the heart's activity during daily activities.
- Event recorder. This portable ECG device is worn for up to 30 days or until an arrhythmia or symptoms occur. You typically press a button when symptoms occur.
- Echocardiogram. This test uses sound waves to take pictures of the beating heart. It can show the structure of the heart and heart valves. It can measure the strength of the heart. It also shows how blood flows through the heart.
- Implantable loop recorder. If symptoms are very infrequent, an event recorder may be implanted under the skin in the chest area. The device continuously records the heart's electrical activity. It can find irregular heart rhythms.
If an irregular heartbeat is not found during those tests, a healthcare professional may suggest more tests to try to trigger the arrhythmia. These tests may include:
- Stress test. Some arrhythmias are triggered or worsened by exercise. During a stress test, the heart's activity is watched while you ride on a stationary bicycle or walk on a treadmill. If you can't exercise, you may be given medicine that affects the heart in a way that's similar to exercise.
- Tilt table test. This test may be done if you've had fainting spells. Your heart rate and blood pressure are checked as you lie flat on a table. The table is then tilted to put you in a standing position. A healthcare professional watches how your heart and nervous system respond to the change in angle.
Electrophysiological (EP) testing and mapping. This test, also called an EP study, can confirm a diagnosis of tachycardia or find out where in the heart the faulty signaling occurs. An EP study is mostly used to diagnose isolated arrythmias.
An EP study is done in the hospital. One or more thin, flexible tubes are guided through a blood vessel, usually in the groin, to various areas in the heart. Sensors on the tips of the tubes record the heart's electrical activity. An EP study shows how electrical signals spread through the heart during each heartbeat.
More Information
Treatment
Treatment for a heart arrhythmia depends on whether the heart is beating too fast or too slow. Some heart arrhythmias do not need treatment. Your healthcare team may suggest regular checkups to watch your condition.
Heart arrhythmia treatment is usually only needed if the irregular heartbeat causes significant symptoms or puts you at risk of more-serious heart problems. Treatment for heart arrhythmias may include medicines, special actions called vagal maneuvers, procedures or surgery.
Medicines
Medicines used to treat heart arrhythmias depend on the type of irregular heartbeat and possible complications.
For example, most people with tachycardia are given medicine to control the heart rate and rhythm.
If you have atrial fibrillation, blood thinners may be given to prevent blood clots.
Therapies
Other treatments for heart arrhythmias include:
- Vagal maneuvers. These are simple but specific actions that can slow the heart rate. They include coughing, bearing down as if having a bowel movement and putting an ice pack on the face. These actions affect the vagus nerve. The nerve helps control the heartbeat. Vagal maneuvers may be recommended if you have a very fast heartbeat due to supraventricular tachycardia. Vagal maneuvers don't work for all types of arrhythmias.
- Cardioversion. Paddles or patches on the chest are used to give an electrical shock to the heart and help reset the heart rhythm. Cardioversion is typically used when vagal maneuvers and medicines don't work. Your healthcare team may recommend this treatment if you have a certain type of arrhythmia, such as atrial fibrillation.
Surgery or other procedures
Cardiac catheter ablation

Cardiac catheter ablation
In catheter ablation, one or more thin, flexible tubes called catheters are passed through a blood vessel and guided to the heart. Sensors on the catheter tips use heat or extreme cold to scar a small area of heart tissue. The scarring blocks faulty electrical signals that cause an irregular heartbeat.
Pacemakers, defibrillator
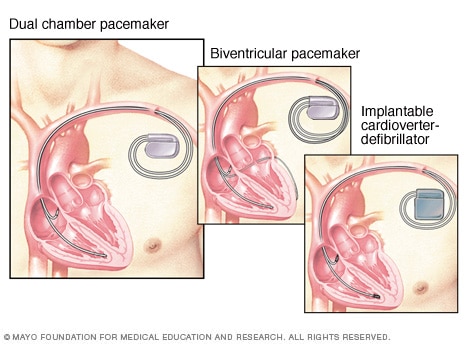
Pacemakers, defibrillator
A pacemaker helps the heart keep a steady beat. If the device finds a slow heartbeat, it sends electrical signals to correct the beat. A dual chamber pacemaker checks, or paces, the heart signals in the right upper and lower heart chambers. A biventricular pacemaker paces both lower heart chambers. An implantable cardioverter-defibrillator (ICD) continuously checks for irregular heartbeats. If it finds one, it sends a brief shock to reset the heart rhythm.
Treatment for heart arrhythmias also may involve a procedure or surgery to place a heart device in your body. Sometimes, open-heart surgery is needed to stop or prevent an irregular heartbeat.
Types of procedures and surgeries used to treat heart arrhythmias include:
- Catheter ablation. In this procedure, the doctor places one or more catheters into blood vessels to the heart. Sensors at the catheter tips use heat or cold energy to create tiny scars in your heart. The scars block irregular heart signals and restore the heartbeat.
- Pacemaker. If slow heartbeats don't have a cause that can be fixed, a pacemaker may be needed. A pacemaker is a small device that's placed in the chest to help control the heartbeat.
Implantable cardioverter-defibrillator (ICD). This device is placed under the skin near the collarbone. It continuously checks the heart rhythm. If the device finds an irregular heartbeat, it sends out low- or high-energy shocks to reset the heart's rhythm.
You may need this device if you have a high risk of dangerously fast or irregular heartbeats in the lower heart chambers. Such conditions are called ventricular tachycardia or ventricular fibrillation. Other reasons for an ICD include a history of sudden cardiac arrest or conditions that increase its risk.
Maze procedure. In the maze procedure, a surgeon makes tiny cuts in the upper half of the heart to create a pattern of scar tissue. The pattern is called a maze. The heart's signals can't pass through scar tissue. This treatment can block stray electrical heart signals that cause some types of fast heartbeats.
The maze procedure is usually only done if you don't get better with other treatments or if you're already having open-heart surgery for another reason.
- Coronary bypass graft surgery. If you have severe coronary artery disease with an irregular heartbeat, you may need this type of heart surgery. The surgery creates a new path for blood to flow around a blocked or partially blocked artery in the heart.
After treatment for irregular heartbeats, it's important to get regular health checkups. Take your medicines as directed. Tell your healthcare team if your symptoms get worse.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Making lifestyle changes can help keep your heart as healthy as possible.
Examples of heart-healthy lifestyle changes are:
- Eat heart-healthy foods. Eat a healthy diet that's low in salt and solid fats and rich in fruits, vegetables and whole grains.
- Get regular exercise. Try to exercise for at least 30 minutes on most days.
- Don't smoke. If you smoke and can't quit on your own, talk to a healthcare professional about strategies or programs to help.
- Maintain a healthy weight. Being overweight increases the risk of heart disease. Talk with your care team to set realistic goals for body mass index (BMI) and weight.
- Control blood pressure and cholesterol. High blood pressure and high cholesterol increase the risk of heart disease. Make lifestyle changes and take medicines as directed to manage high blood pressure or high cholesterol.
- Limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to a healthcare professional about strategies that might help.
- Manage stress. Managing stress is an important step in keeping the heart healthy. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce and manage stress.
Preparing for your appointment
Medical appointments can be brief. There's often a lot to discuss. So it's a good idea to be prepared for your appointment. Here's some information to help you prepare for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance. For example, you may be told not to eat or drink for a few hours before a cholesterol test.
- Write down any symptoms you're having, including any that may seem unrelated to heart arrhythmias.
- Write down important personal information, including a family history of heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medicines, including vitamins or supplements that you're taking. Include dosages.
- Take someone with you, if possible. Someone who goes with you can help you remember information you're given.
- Write down questions to ask your care team.
Prepare a list of questions from most important to least important in case time runs out. For heart arrhythmias, some basic questions to ask your healthcare team include:
- What's the most likely cause of my symptoms?
- Are there other possible causes for my symptoms?
- What kinds of tests will I need? Do I need to do anything to prepare for these tests?
- What's the most appropriate treatment?
- Are there any foods or drinks I should avoid? Is there anything I should add to my diet?
- What's an appropriate level of physical activity?
- How often should I be screened for heart disease or other complications of an arrhythmia?
- I have other health conditions. How can I best manage these conditions together?
- Is there a generic option to the medicine you're prescribing?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
What to expect from your doctor
Your healthcare team is likely to ask you questions, such as:
- When did you first begin having symptoms?
- Do you always have symptoms, or do they come and go?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, makes your symptoms worse?
- Does anyone in your family have a heart arrhythmia?
Mayo Clinic Heart Rhythm Program
Arizona
Florida
Minnesota
Oct. 13, 2023