Overview
Hashimoto's disease is an autoimmune disorder affecting the thyroid gland. The thyroid is a butterfly-shaped gland located at the base of the neck just below the Adam's apple. The thyroid produces hormones that help regulate many functions in the body.
An autoimmune disorder is an illness caused by the immune system attacking healthy tissues. In Hashimoto's disease, immune-system cells lead to the death of the thyroid's hormone-producing cells. The disease usually results in a decline in hormone production (hypothyroidism).
Although anyone can develop Hashimoto's disease, it's most common among middle-aged women. The primary treatment is thyroid hormone replacement.
Hashimoto's disease is also known as Hashimoto's thyroiditis, chronic lymphocytic thyroiditis and chronic autoimmune thyroiditis.
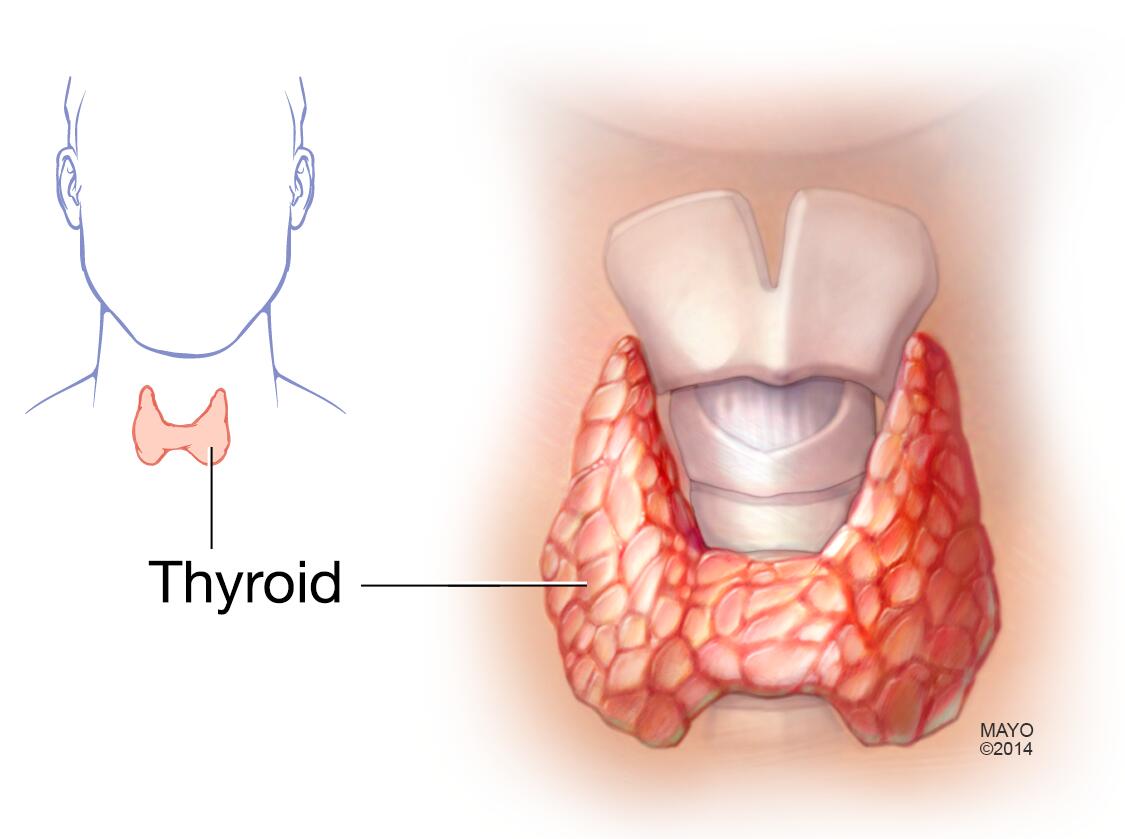
Thyroid gland
The thyroid gland is located at the base of the neck, just below the Adam's apple.
Symptoms
Hashimoto's disease progresses slowly over the years. You may not notice signs or symptoms of the disease. Eventually, the decline in thyroid hormone production can result in any of the following:
- Fatigue and sluggishness
- Increased sensitivity to cold
- Increased sleepiness
- Dry skin
- Constipation
- Muscle weakness
- Muscle aches, tenderness and stiffness
- Joint pain and stiffness
- Irregular or excessive menstrual bleeding
- Depression
- Problems with memory or concentration
- Swelling of the thyroid (goiter)
- A puffy face
- Brittle nails
- Hair loss
- Enlargement of the tongue
When to see a doctor
Signs and symptoms of Hashimoto's disease vary widely and are not specific to the disorder. Because these symptoms could result from any number of disorders, it's important to see your health care provider as soon as possible for a timely and accurate diagnosis.
From Mayo Clinic to your inbox
Causes
Hashimoto's disease is an autoimmune disorder. The immune system creates antibodies that attack thyroid cells as if they were bacteria, viruses or some other foreign body. The immune system wrongly enlists disease-fighting agents that damage cells and lead to cell death.
What causes the immune system to attack thyroid cells is not clear. The onset of disease may be related to:
- Genetic factors
- Environmental triggers, such as infection, stress or radiation exposure
- Interactions between environmental and genetic factors
Risk factors
The following factors are associated with an increased risk of Hashimoto's disease:
- Sex. Women are much more likely to get Hashimoto's disease.
- Age. Hashimoto's disease can occur at any age but more commonly occurs during middle age.
- Other autoimmune disease. Having another autoimmune disease — such as rheumatoid arthritis, type 1 diabetes or lupus — increases your risk of developing Hashimoto's disease.
- Genetics and family history. You're at higher risk for Hashimoto's disease if others in your family have thyroid disorders or other autoimmune diseases.
- Pregnancy. Typical changes in immune function during pregnancy may be a factor in Hashimoto's disease that begins after pregnancy.
- Excessive iodine intake. Too much iodine in the diet may function as a trigger among people already at risk for Hashimoto's disease.
- Radiation exposure. People exposed to excessive levels of environmental radiation are more prone to Hashimoto's disease.
Complications
Thyroid hormones are essential for the healthy function of many body systems. Therefore, when Hashimoto's disease and hypothyroidism are left untreated, many complications can occur. These include:
- Goiter. A goiter is enlargement of the thyroid. As thyroid hormone production declines due to Hashimoto's disease, the thyroid receives signals from the pituitary gland to make more. This cycle may result in a goiter. It's generally not uncomfortable, but a large goiter can affect your appearance and may interfere with swallowing or breathing.
- Heart problems. Hypothyroidism can result in poor heart function, an enlarged heart and irregular heartbeats. It can also result in high levels of low-density lipoprotein (LDL) cholesterol — the "bad" cholesterol — that is a risk factor for cardiovascular disease and heart failure.
- Mental health issues. Depression or other mental health disorders may occur early in Hashimoto's disease and may become more severe over time.
- Sexual and reproductive dysfunction. In women, hypothyroidism can result in a reduced sexual desire (libido), an inability to ovulate, and irregular and excessive menstrual bleeding. Men with hypothyroidism may have a reduced libido, erectile dysfunction and a lowered sperm count.
- Poor pregnancy outcomes. Hypothyroidism during pregnancy may increase the risk of a miscarriage or preterm birth. Babies born to women with untreated hypothyroidism are at risk for decreased intellectual abilities, autism, speech delays and other developmental disorders.
- Myxedema (miks-uh-DEE-muh). This rare, life-threatening condition can develop due to long-term, severe, untreated hypothyroidism. Its signs and symptoms include drowsiness followed by profound lethargy and unconsciousness. A myxedema coma may be triggered by exposure to cold, sedatives, infection or other stress on your body. Myxedema requires immediate emergency medical treatment.