Diagnosis
Upper endoscopy
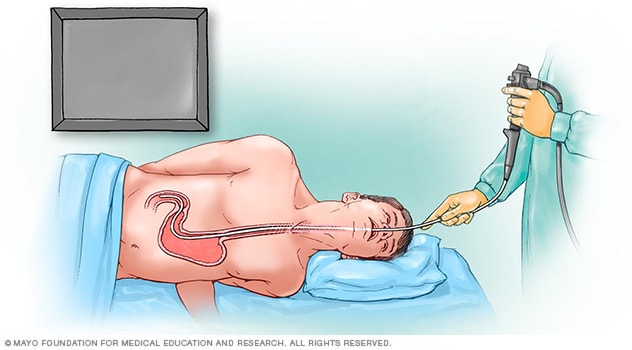
Upper endoscopy
An upper endoscopy procedure involves passing a long, flexible tube called an endoscope down the throat and into the esophagus. A tiny camera on the end of the endoscope lets a medical specialist to examine the esophagus, stomach and the beginning of the small intestine, called the duodenum.
To find the cause of gastrointestinal bleeding, a health care professional will first take your medical history, including a history of previous bleeding, and do a physical exam. Tests also may be ordered, such as:
- Blood tests. You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests.
- Stool tests. Analyzing your stool can help determine the cause of occult bleeding.
- Nasogastric lavage. A tube is passed through your nose into the stomach to remove stomach contents. This might help find the source of the bleeding.
- Upper endoscopy. An upper endoscopy is a procedure that uses a camera to view the upper digestive system. The camera is attached to a long, thin tube, called an endoscope, and passed down the throat to examine the upper gastrointestinal tract.
- Colonoscopy. During a colonoscopy, a long, flexible tube is inserted into the rectum. A tiny video camera at the tip of the tube allows the doctor to view the inside of the entire large intestine and rectum.
- Capsule endoscopy. In this procedure, you swallow a vitamin-size capsule with a tiny camera inside. The capsule travels through your digestive tract taking thousands of pictures that are sent to a recorder you wear on a belt around your waist.
- Flexible sigmoidoscopy. A tube with a light and camera is placed in the rectum to look at the rectum and the last part of the large intestine, known as the sigmoid colon.
- Balloon-assisted enteroscopy. A specialized scope inspects parts of the small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test.
- Angiography. A contrast dye is injected into an artery, and a series of X-rays are taken to look for and treat bleeding vessels or other issues.
- Imaging tests. A variety of other imaging tests, such as a CT scan of the belly, might be used to find the source of the bleed.
If your GI bleeding is severe, and noninvasive tests can't find the source, you might need surgery so that doctors can view the entire small intestine. Fortunately, this is rare.
Treatment
GI bleeding often stops on its own. If it doesn't, treatment depends on where the bleed is from. In many cases, bleeding can be treated with medicine or a procedure during a test. For example, it's sometimes possible to treat a bleeding peptic ulcer during an upper endoscopy or to remove polyps during a colonoscopy.
If you have an upper GI bleed, you will be given an IV drug known as a proton pump inhibitor (PPI) to suppress stomach acid production. Once the source of the bleeding is identified, your doctor will determine whether you need to continue taking a PPI.
Depending on the amount of blood loss and whether you continue to bleed, you might need fluids through a needle (IV) and, possibly, blood transfusions. If you take blood-thinning medicines, including aspirin or nonsteroidal anti-inflammatory medications, you might need to stop.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
If your bleeding is not severe, you might start by seeing your doctor or other general health care professional. Or you might be referred immediately to a specialist in gastrointestinal disorders, called a gastroenterologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment and when they began.
- All medicines, vitamins or other supplements you take, including doses.
- History of digestive disease you've been diagnosed with, such as GERD, peptic ulcers or IBD.
- Questions to ask during your appointment.
Take a family member or friend along, if possible, to help you remember the information you're given.
For gastrointestinal bleeding, basic questions to ask include:
- I'm not seeing blood, so why do you suspect a GI bleed?
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- What are the alternatives to the primary approach you're suggesting?
- I have other health conditions. How can I best manage them while my bleeding is treated?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
You'll likely be asked a few questions, such as:
- Have your symptoms been constant? Or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you take nonsteroidal anti-inflammatory medicine, either nonprescription or prescribed, or do you take aspirin?
- Do you drink alcohol?
Oct. 13, 2023