Diagnosis
You might first notice a fibroadenoma when you bathe or shower. Or you may notice it while you do a breast self-exam. Fibroadenomas also may be found during a regular medical exam, a screening mammogram or a breast ultrasound.
If you have a breast lump that can be felt, you might need certain tests or procedures. Which tests you need depends on your age and the features of the breast lump.
Imaging tests
Imaging tests give details about the size, shape and other features of a breast lump:
- Breast ultrasound uses sound waves to create pictures of the inside of the breast. If you're younger than 30, your provider likely will use breast ultrasound to check a breast lump. Ultrasound clearly shows the size and shape of a fibroadenoma. This test also can show the difference between a solid breast lump and a fluid-filled cyst. An ultrasound causes no pain. Nothing needs to go inside your body for this test.
- Mammography uses X-rays to make an image of breast tissue. This image is called a mammogram. It detects the borders of a fibroadenoma and sets it apart from other tissues. But mammography might not be the best imaging test to use for fibroadenomas in younger people, who can have dense breast tissue. Dense tissue makes it harder to see the difference between typical breast tissue and what might be a fibroadenoma. Also, due to the risk of radiation from mammograms, they are generally not used to check breast lumps in people under age 30.
Biopsy
Core needle biopsy
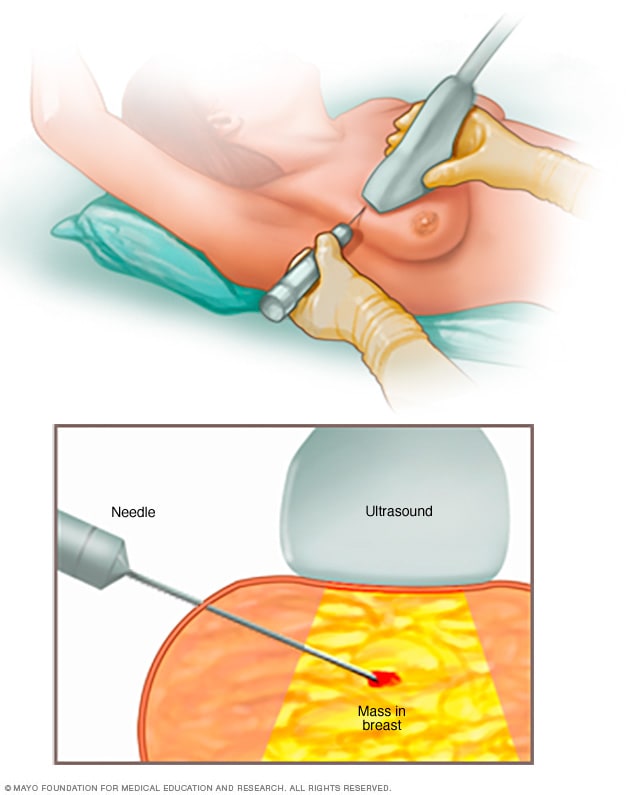
Core needle biopsy
A core needle biopsy uses a long, hollow tube to obtain a sample of tissue. Here, a biopsy of a suspicious breast lump is being done. The sample is sent to a lab for testing by doctors called pathologists. They specialize in examining blood and body tissue.
If there's any question about the type or nature of the breast lump, you may need a test called a biopsy to check a sample of the tissue. A common biopsy method for a fibroadenoma is a core needle biopsy.
A doctor called a radiologist usually performs a core needle biopsy. An ultrasound device helps the doctor guide the needle to the right spot. A special, hollow needle collects a tiny sample of breast tissue. A lab exam of the sample can reveal what kind of lump is present. A doctor called a pathologist reviews the sample to see if it is a fibroadenoma or phyllodes tumor.
If the breast lump is growing quickly, or causing pain or other problems, you may need to have the entire lump removed. This might also happen if the biopsy results are not clear. A surgeon will talk with you about your options.
Treatment
Often, fibroadenomas need no treatment. But, in some cases, you may need surgery to remove a fast-growing fibroadenoma.
When no treatment is needed
If results of an imaging test and biopsy show that your breast lump is a fibroadenoma, you may not need surgery to remove it.
When deciding about surgery, keep these things in mind:
- Surgery can change the appearance of your breast.
- Fibroadenomas sometimes shrink or go away on their own.
- Fibroadenomas may remain as they are with no change.
If you decide not to have surgery, your provider may advise follow-up visits to watch the fibroadenoma. At these visits, you may have an ultrasound to check for changes in the shape or size of the breast lump. In between visits, let your provider know if you notice any changes in your breasts.
When you may need surgery
If results from an imaging test or biopsy are concerning to your provider, you may need surgery. You may also need surgery if the fibroadenoma is large, grows quickly or causes symptoms. Surgery is the standard treatment for giant fibroadenomas and phyllodes tumors.
Procedures to remove a fibroadenoma include:
- Cutting it out. In this procedure, a surgeon uses a knife to remove the entire fibroadenoma. This is called surgical excision.
- Freezing it. In this procedure, a thin device shaped like a wand is inserted through the skin of the breast to the fibroadenoma. The device gets very cold and freezes the tissue. This destroys the fibroadenoma. This technique is not available at all medical centers.
After treatment, other fibroadenomas can form. If you find a new breast lump, tell your health care provider. You may need testing with ultrasound, mammography or biopsy to see whether the new breast lump is a fibroadenoma or another breast condition.
Preparing for your appointment
You may first see your usual health care provider for concerns about a breast lump. Or you may go to a doctor who specializes in conditions that affect the female reproductive system. This doctor is a gynecologist. Here's what you need to know to get ready for your appointment.
What you can do
When you make the appointment, ask whether you need to do anything before you arrive. For example, should you stop taking any medications in case you need a biopsy. Make a list of:
- Your symptoms, including even those that don't seem to be related to your breast changes. Note when they began.
- Key personal information, including your medical history and whether you have a history of breast cancer in your family.
- All medications, vitamins or other supplements you take, including doses.
- Questions to ask your health care provider.
For a fibroadenoma, ask basic questions such as:
- What might this lump be?
- What tests do I need? Do I need to do anything special to prepare for them?
- Will I need treatment?
- Do you have brochures or other written materials about this topic? What websites do you suggest I use for more information?
Be sure to ask other questions as you think of them. If you can, bring a family member or friend along to your appointment. That person may help you remember the information you're given.
What to expect from your provider
Your health care provider is likely to ask you a number of questions, such as:
- When did you first notice the breast lump? Has its size changed?
- Are there changes in the breast lump before or after your period?
- Have you or other family members had breast problems?
- What date did your last period begin?
- Is the breast lump tender or painful?
- Do you have fluid leaking from your nipple?
- Have you ever had a mammogram? If so, when?
Oct. 13, 2022