Overview
End-stage renal disease, also called end-stage kidney disease or kidney failure, occurs when chronic kidney disease — the gradual loss of kidney function — reaches an advanced state. In end-stage renal disease, your kidneys no longer work as they should to meet your body's needs.
Your kidneys filter wastes and excess fluids from your blood, which are then excreted in your urine. When your kidneys lose their filtering abilities, dangerous levels of fluid, electrolytes and wastes can build up in your body.
With end-stage renal disease, you need dialysis or a kidney transplant to stay alive. But you can also choose to opt for conservative care to manage your symptoms — aiming for the best quality of life during your remaining time.
One of the important jobs of the kidneys is to clean the blood. As blood moves through the body, it picks up extra fluid, chemicals and waste. The kidneys separate this material from the blood. It's carried out of the body in urine. If the kidneys are unable to do this and the condition is untreated, serious health problems result, with eventual loss of life.
Products & Services
Symptoms
Early in chronic kidney disease, you might have no signs or symptoms. As chronic kidney disease progresses to end-stage renal disease, signs and symptoms might include:
- Nausea
- Vomiting
- Loss of appetite
- Fatigue and weakness
- Changes in how much you urinate
- Chest pain, if fluid builds up around the lining of the heart
- Shortness of breath, if fluid builds up in the lungs
- Swelling of feet and ankles
- High blood pressure (hypertension) that's difficult to control
- Headaches
- Difficulty sleeping
- Decreased mental sharpness
- Muscle twitches and cramps
- Persistent itching
- Metallic taste
Signs and symptoms of kidney disease are often nonspecific, meaning they can also be caused by other illnesses. Because your kidneys can make up for lost function, signs and symptoms might not appear until irreversible damage has occurred.
When to seek care
Make an appointment with your health care provider if you have signs or symptoms of kidney disease.
If you have a medical condition that increases your risk of kidney disease, your care provider is likely to monitor your kidney function with urine and blood tests and your blood pressure during regular office visits. Ask your provider whether these tests are necessary for you.
Causes
Healthy kidney vs. diseased kidney
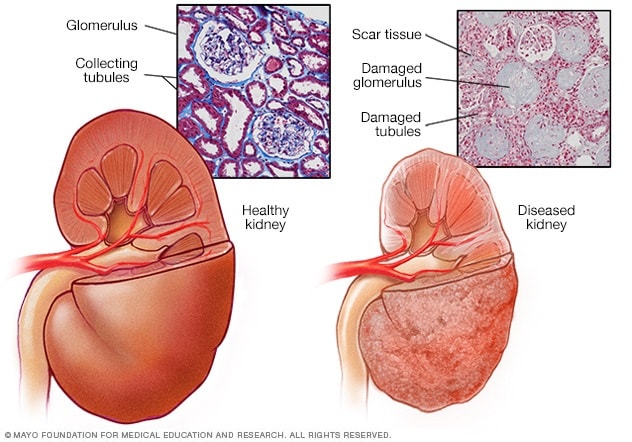
Healthy kidney vs. diseased kidney
A typical kidney has about 1 million filtering units. Each unit, called a glomerulus, joins a tubule. The tubule collects urine. Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring.
Polycystic kidney
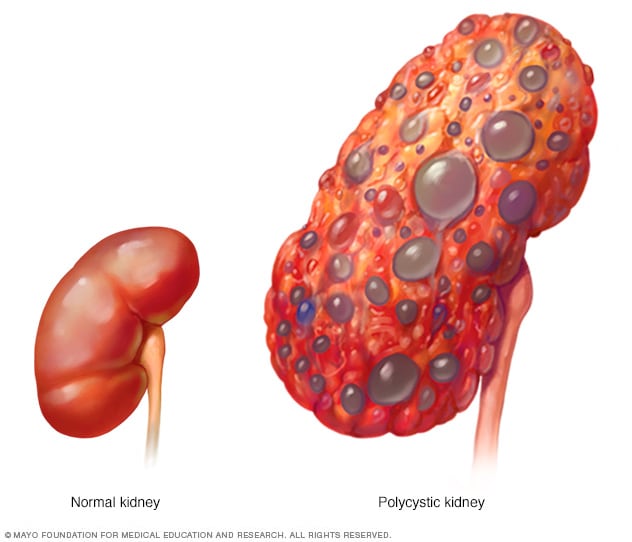
Polycystic kidney
A healthy kidney (left) removes waste from the blood and maintains the body's chemical balance. With polycystic kidney disease (right), fluid-filled sacs called cysts develop in the kidneys. The kidneys grow larger and slowly lose their ability to work as they should.
Kidney disease occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years. For some people, kidney damage can continue to progress even after the underlying condition is resolved.
Diseases and conditions that can lead to kidney disease include:
- Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis) — an inflammation of the kidney's filtering units (glomeruli)
- Interstitial nephritis (in-tur-STISH-ul nuh-FRY-tis), an inflammation of the kidney's tubules and surrounding structures
- Polycystic kidney disease or other inherited kidney diseases
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis (pie-uh-low-nuh-FRY-tis)
Risk factors
Certain factors increase the risk that chronic kidney disease will progress more quickly to end-stage renal disease, including:
- Diabetes with poor blood sugar control
- Kidney disease that affects the glomeruli, the structures in the kidneys that filter wastes from the blood
- Polycystic kidney disease
- High blood pressure
- Tobacco use
- Black, Hispanic, Asian, Pacific Islander or American Indian heritage
- Family history of kidney failure
- Older age
- Frequent use of medications that could be damaging to the kidney
Complications
Kidney damage, once it occurs, can't be reversed. Potential complications can affect almost any part of your body and can include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart's ability to function and may be life-threatening
- Heart disease
- Weak bones and an increased risk of bone fractures
- Anemia
- Decreased sex drive, erectile dysfunction or reduced fertility
- Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures
- Decreased immune response, which makes you more vulnerable to infection
- Pericarditis, an inflammation of the saclike membrane that envelops your heart (pericardium)
- Pregnancy complications that carry risks for the mother and the developing fetus
- Malnutrition
- Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival
Prevention
If you have kidney disease, you may be able to slow its progress by making healthy lifestyle choices:
- Achieve and maintain a healthy weight
- Be active most days
- Limit protein and eat a balanced diet of nutritious, low-sodium foods
- Control your blood pressure
- Take your medications as prescribed
- Have your cholesterol levels checked every year
- Control your blood sugar level
- Don't smoke or use tobacco products
- Get regular checkups
Oct. 10, 2023