Overview
Chronic obstructive pulmonary disease (COPD) is an ongoing lung condition caused by damage to the lungs. The damage results in swelling and irritation, also called inflammation, inside the airways that limit airflow into and out of the lungs. This limited airflow is known as obstruction. Symptoms include trouble breathing, a daily cough that brings up mucus and a tight, whistling sound in the lungs called wheezing.
COPD is most often caused by long-term exposure to irritating smoke, fumes, dust or chemicals. The most common cause is cigarette smoke.
Emphysema and chronic bronchitis are the two most common types of COPD. These two conditions usually occur together and can vary in severity among people with COPD.
Chronic bronchitis is inflammation of the lining of the tubes that bring air into the lungs. These tubes are called bronchi. The inflammation prevents good airflow into and out of the lungs and makes extra mucus. In emphysema, the small air sacs of the lungs, called alveoli, are damaged. The damaged alveoli can't pass enough oxygen into the bloodstream.
Although COPD is a condition that can get worse over time, COPD is treatable. With proper management, most people with COPD can control symptoms and improve their quality of life. Proper management also can lower the risk of other conditions linked to COPD, such as heart disease and lung cancer.
Products & Services
Symptoms
COPD symptoms often don't appear until a lot of lung damage has occurred. Symptoms usually worsen over time, especially if smoking or other irritating exposure continues.
Symptoms of COPD may include:
- Trouble catching your breath, especially during physical activities.
- Wheezing or whistling sounds when breathing.
- Ongoing cough that may bring up a lot of mucus. The mucus may be clear, white, yellow or greenish.
- Chest tightness or heaviness.
- Lack of energy or feeling very tired.
- Frequent lung infections.
- Losing weight without meaning to. This may happen as the condition worsens.
- Swelling in ankles, feet or legs.
People with COPD also are likely to have times when their symptoms become worse than the usual day-to-day variation. This time of worsening symptoms is called an exacerbation (eg-zas-er-bay-shun). Exacerbations can last for several days to weeks. They can be caused by triggers such as smells, cold air, air pollution, colds or infections. Symptoms may include:
- Working harder than usual to breathe or having trouble breathing.
- Chest tightness.
- Coughing more often.
- More mucus or changes in mucus color or thickness.
- Fever.
When to see a doctor
Talk with your doctor or other healthcare professional if your symptoms don't get better with treatment or if symptoms get worse. Also talk with your healthcare professional if you notice symptoms of an infection, such as fever or a change in the mucus you cough up.
In the U.S., call 911 or your local emergency number for help or go to the emergency department at a hospital right away if you can't catch your breath, your lips or fingernail beds are blue, you have a fast heartbeat, or you feel foggy and have trouble concentrating.
Causes
The main cause of COPD in developed countries is tobacco smoking. In the developing world, COPD often occurs in people exposed to fumes from burning fuel for cooking and heating in homes that don't have good airflow. Long-term exposure to chemical fumes, vapors and dusts in the workplace is another cause of COPD.
Not all people who have smoked for a long time have COPD symptoms, but they may still have lung damage, so their lungs don't work as well as they used to. Some people who smoke get less common lung conditions that may be diagnosed as COPD until a more thorough exam shows a different diagnosis.
How the lungs are affected
Air travels down the windpipe called the trachea and into the lungs through two large tubes called bronchi. Inside the lungs, these tubes divide many times like the branches of a tree. Many smaller tubes called bronchioles end in clusters of tiny air sacs called alveoli.
The alveoli have very thin walls full of tiny blood vessels. The oxygen in the air breathed in passes into these blood vessels and goes into the bloodstream. At the same time, carbon dioxide, a gas that is a waste product from the body, passes into the alveoli and is breathed out.
When breathing out, the natural stretchiness of the alveoli forces old air out, allowing new air to get in. This stretchiness is also called elasticity.
Causes of airway obstruction
Emphysema
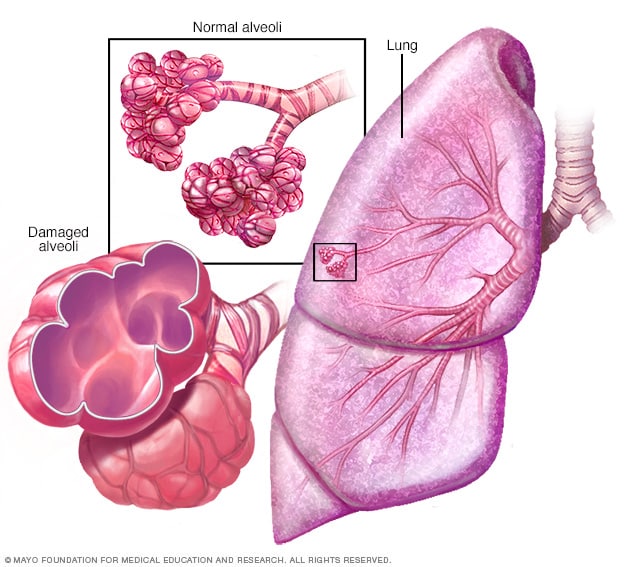
Emphysema
In emphysema, the inner walls of the lungs' air sacs called alveoli are damaged, causing them to eventually rupture. This creates one larger air space instead of many small ones and reduces the surface area available for gas exchange.
Bronchitis
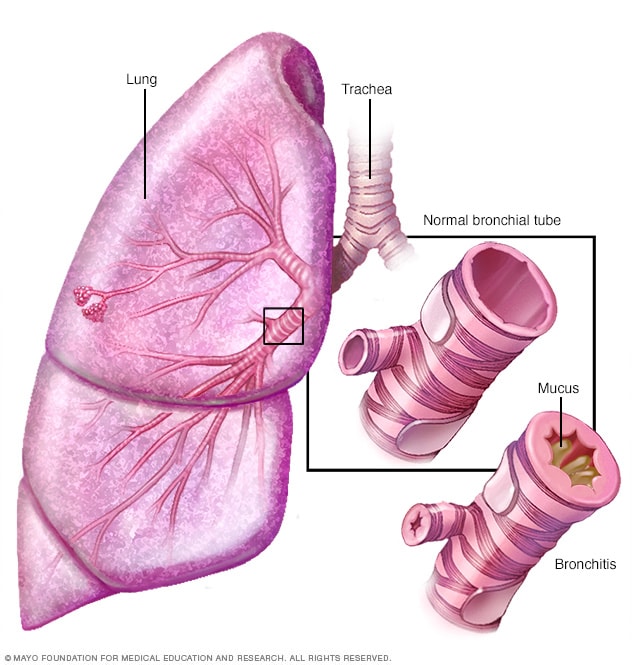
Bronchitis
Bronchitis is an inflammation of the lining of the bronchial tubes, which carry air to and from the lungs. People who have bronchitis often cough up thickened mucus, which can be discolored.
Long-term exposure to irritants, such as from smoking, injures the lungs. This damage keeps air from moving in and out of the lungs freely, limiting their ability to provide oxygen to the bloodstream and take away carbon dioxide. The two main conditions that prevent effective airflow in the lungs are:
- Emphysema. This lung condition causes destruction of the fragile walls and elastic fibers of the alveoli. The damaged inner walls of the alveoli may be destroyed, creating one large air space that is hard to empty compared with the many healthy small ones. The alveoli now have less surface area that can be used to exchange oxygen and carbon dioxide. Also, old air gets trapped in the large alveoli so there isn't room for enough new air to get in.
- Chronic bronchitis. In this condition, the bronchial tubes become inflamed and narrowed. As a result, the tubes thicken, making less room for air to pass through. Extra mucus caused by the irritation blocks the narrowed tubes even more. An ongoing cough results from trying to clear mucus from the airways.
Cigarette smoke and other irritants
In the vast majority of people with COPD in the United States, the lung damage that leads to COPD is caused by long-term cigarette smoking. But there are likely other factors at play in developing COPD because not everyone who smokes gets COPD. One such factor may be gene changes that make some people more likely to develop the condition.
Other irritants can cause COPD, including cigar smoke, secondhand smoke, pipe smoke, air pollution, and workplace exposure to dust, smoke or fumes.
Alpha-1-antitrypsin deficiency
In about 1% of people with COPD, the condition results from a gene change passed down in families. This is a genetic form of emphysema. This gene lessens the levels of a protein called alpha-1-antitrypsin (AAT) in the body. AAT is made in the liver and released into the bloodstream to help protect the lungs from damage caused by smoke, fumes and dust.
Low levels of this protein, a condition called alpha-1-antitrypsin (AAT) deficiency, can cause liver damage, lung conditions such as COPD or both. With AAT deficiency, there is usually a family history of COPD, and symptoms begin at a younger age.
Risk factors
Risk factors for COPD include:
- Tobacco smoke. The biggest risk factor for COPD is long-term cigarette smoking. The more years you smoke and the more packs you smoke, the greater your risk. Pipe, cigar and marijuana smoking also may raise your risk. People who breathe in large amounts of secondhand smoke are at risk of COPD too.
- Asthma. Asthma is a condition in which the airways narrow and swell and may produce extra mucus. Asthma may be a risk factor for developing COPD. The mix of asthma and smoking raises the risk of COPD even more.
- Workplace exposure. Long-term exposure to chemical fumes, smoke, vapors and dusts in the workplace can irritate and cause swelling in the lungs. This can raise the risk of COPD.
- Fumes from burning fuel. In the developing world, people exposed to fumes from burning fuel for cooking and heating in homes with poor airflow are at higher risk of COPD.
- Genetics. AAT deficiency caused by a gene change passed down in families is the cause of COPD in some people. This genetic form of emphysema is not common. Other genetic factors may make certain people who smoke more likely to get COPD.
Complications
COPD can cause many complications, including:
- Respiratory infections. People with COPD are more likely to have colds, the flu and pneumonia. Any respiratory infection can make it much harder to breathe and could cause more damage to lung tissue.
- Heart problems. For reasons that aren't fully understood, COPD can raise the risk of heart disease, including heart attack.
- Lung cancer. People with COPD have a higher risk of getting lung cancer.
- High blood pressure in lung arteries. COPD may cause high blood pressure in the arteries that bring blood to the lungs. This condition is called pulmonary hypertension.
- Anxiety and depression. Difficulty breathing can keep you from doing activities that you enjoy. And having a serious medical condition such as COPD can sometimes cause anxiety and depression.
Prevention
Unlike some other medical conditions, COPD often has a clear cause and a clear way to prevent it. Most of the time, COPD is directly linked to cigarette smoking. The best way to prevent COPD is to never smoke. If you smoke and have COPD, stopping now can slow how fast the condition worsens.
If you've smoked for a long time, quitting can be hard, especially if you've tried quitting once, twice or many times before. But keep trying to quit. It's critical to find a stop-smoking program that can help you quit for good. It's your best chance for lessening damage to your lungs. Talk with your healthcare professional about options that might work best for you.
Workplace exposure to chemical fumes, vapors and dusts is another risk factor for COPD. If you work with these types of lung irritants, talk with your supervisor about the best ways to protect yourself. This may include wearing equipment that prevents you from breathing in these substances.
Here are some steps you can take to help prevent complications linked with COPD:
- Quit smoking to help lower your risk of heart disease and lung cancer.
- Get an annual flu vaccination and vaccination against pneumococcal pneumonia to lower your risk of or prevent some infections. Also talk with your doctor or other healthcare professional about when you need the COVID-19 vaccine and the RSV vaccine.
- Talk with your healthcare professional or a mental health professional if you feel sad or hopeless or think that you may have depression.
Aug. 30, 2024