Overview
Alzheimer's disease is the most common cause of dementia. Alzheimer's disease is the biological process that begins with the appearance of a buildup of proteins in the form of amyloid plaques and neurofibrillary tangles in the brain. This causes brain cells to die over time and the brain to shrink.
About 6.9 million people in the United States age 65 and older live with Alzheimer's disease. Among them, more than 70% are age 75 and older. Of the more than 55 million people in the world with dementia, 60% to 70% are estimated to have Alzheimer's disease.
Early symptoms of Alzheimer's disease include forgetting recent events or conversations. Over time, Alzheimer's disease leads to serious memory loss and affects a person's ability to do everyday tasks.
There is no cure for Alzheimer's disease. In advanced stages, loss of brain function can cause dehydration, poor nutrition or infection. These complications can result in death.
But medicines may improve symptoms or slow the decline in thinking. Programs and services can help support people with the disease and their caregivers.
Products & Services
Symptoms
Memory loss is the key symptom of Alzheimer's disease. Early in the disease, people may have trouble remembering recent events or conversations. Over time, memory gets worse and other symptoms occur.
At first, someone with the disease may be aware of having trouble remembering things and thinking clearly. As signs and symptoms get worse, a family member or friend may be more likely to notice the issues.
Brain changes from Alzheimer's disease lead to the following symptoms that get worse over time.
Memory
Everyone has trouble with memory at times, but the memory loss related to Alzheimer's disease is lasting. Over time, memory loss affects the ability to function at work and at home.
People with Alzheimer's disease may:
- Repeat statements and questions over and over.
- Forget conversations, appointments or events.
- Misplace items, often putting them in places that don't make sense.
- Get lost in places they used to know well.
- Forget the names of family members and everyday objects.
- Have trouble finding the right words, expressing thoughts or having conversations.
Thinking and reasoning
Alzheimer's disease causes trouble concentrating and thinking, especially about abstract concepts such as numbers. Doing more than one task at once is especially hard. It may be challenging to manage finances, balance checkbooks and pay bills on time. Eventually people with Alzheimer's disease may not recognize numbers.
Making judgments and decisions
Alzheimer's disease makes it hard to make sensible decisions and judgments. People with Alzheimer's disease may make poor choices in social settings or wear clothes for the wrong type of weather. Everyday problems may be hard to solve. Someone with Alzheimer's disease may not know how to handle food burning on the stove or how to make decisions when driving.
Planning and performing familiar tasks
Routine activities that involve completing steps in a certain order also can be hard for people with Alzheimer's disease. They may have trouble planning and cooking a meal or playing a favorite game. As Alzheimer's disease becomes advanced, people forget how to do basic tasks such as dressing and bathing.
Changes in personality and behavior
Brain changes that occur in Alzheimer's disease can affect moods and behaviors. Symptoms may include:
- Depression.
- Loss of interest in activities.
- Social withdrawal.
- Mood swings.
- Not trusting others.
- Anger or aggression.
- Changes in sleeping habits.
- Wandering.
- Loss of inhibitions.
- Delusions, such as believing something has been stolen when it hasn't.
Preserved skills
Despite major changes to memory and skills, people with Alzheimer's disease are able to keep some skills even as symptoms get worse. These are known as preserved skills. They may include reading or listening to books, telling stories, sharing memories, singing, listening to music, dancing, drawing, or doing crafts.
Preserved skills may last longer because they're managed by parts of the brain affected in later stages of the disease.
When to see a doctor
Several conditions can cause memory loss or other dementia symptoms. Some of those conditions can be treated. If you are concerned about your memory or other thinking skills, talk to your healthcare professional.
If you are concerned about the thinking skills you notice in a family member or friend, ask about going together to talk to a healthcare professional.
More Information
Causes
Healthy brain and brain with Alzheimer's disease
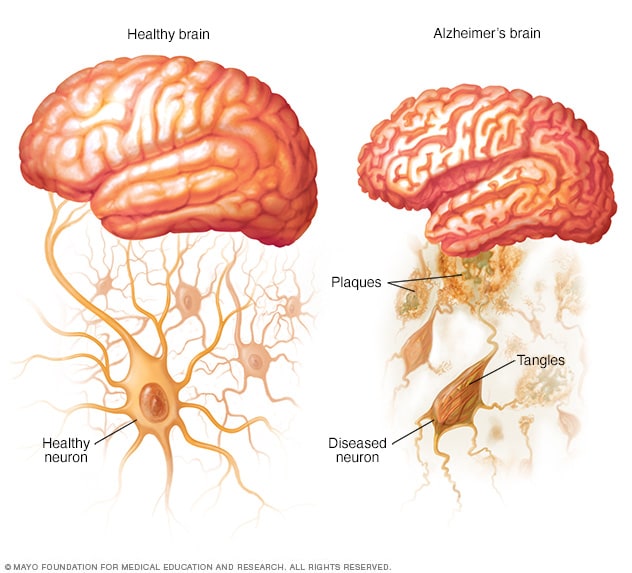
Healthy brain and brain with Alzheimer's disease
In the brain of someone with Alzheimer's disease, amyloid plaques form and tau proteins change shape and become tangles.
The exact causes of Alzheimer's disease aren't fully understood. But at a basic level, brain proteins don't function as usual. This disrupts the work of brain cells, also known as neurons, and triggers a series of events. The neurons become damaged and lose connections to each other. They eventually die.
Scientists believe that for most people, Alzheimer's disease is caused by a combination of genetic, lifestyle and environmental factors that affect the brain over time. In less than 1% of people, Alzheimer's is caused by specific genetic changes that almost guarantee a person will develop the disease. For people in this group, the disease usually begins in middle age.
The disease begins years before the first symptoms. The damage most often starts in the region of the brain that manages memory. The loss of neurons spreads in a somewhat predictable pattern to other regions of the brain. By the late stage of the disease, the brain has shrunk.
Researchers trying to understand the cause of Alzheimer's disease are focused on the role of two proteins:
- Plaques. Beta-amyloid is a fragment of a larger protein. When these fragments clump together, they affect communication between brain cells. The clumps form larger deposits called amyloid plaques.
- Tangles. Tau proteins play a part in a brain cell's internal support and transport system to carry nutrients and other essential materials. In Alzheimer's disease, tau proteins change mshape and organize into structures called neurofibrillary tangles. The tangles disrupt the transport system and cause damage to cells.
Risk factors
Risk factors for Alzheimer's disease include age, family history, lifestyle and other factors.
Older age
Older age is the strongest known risk factor for Alzheimer's disease. Alzheimer's isn't a part of typical aging. But as you grow older, the chances of getting the disease goes up.
One study found that there were four new diagnoses per 1,000 people ages 65 to 74 every year. Among people ages 75 to 84, there were 32 new diagnoses per 1,000 people. For those 85 and older, there were 76 new diagnoses per 1,000 people.
Family history and genetics
The risk of getting Alzheimer's disease is higher if a first-degree relative such as a parent or sibling was diagnosed with the disease. How genes among families affect the risk is largely not understood. The genetic factors are likely complex.
A better understood genetic factor is a form of the apolipoprotein E (APOE) gene. Having the form of the gene known as APOE e4 increases the risk of Alzheimer's disease. About 25% to 30% of the population carries APOE e4. But not everyone with this form of the gene develops the disease. Having two copies of APOE e4 increases the risk of Alzheimer's disease more than having one copy.
Scientists have found rare changes in three genes that virtually guarantee a person who inherits one of them will develop Alzheimer's. But these changes account for less than 1% of people with Alzheimer's disease.
Down syndrome
Many people with Down syndrome develop Alzheimer's disease. This is likely related to having three copies of chromosome 21. Chromosome 21 is the gene involved in the production of the protein that leads to the creation of beta-amyloid. Beta-amyloid fragments can become plaques in the brain. Symptoms tend to appear 10 to 20 years earlier in people with Down syndrome than they do for the general population.
Sex assigned at birth
Overall there are more women with the disease because they tend to live longer than men.
Mild cognitive impairment
Someone with mild cognitive impairment, also called MCI, has a bigger decline in memory or other thinking skills than is usual for the person's age. But the decline doesn't prevent the person from functioning at work or socially.
However, people with MCI have a higher risk of getting dementia than are people who don't have mild cognitive impairment. When MCI affects mainly memory, the condition is more likely to progress to dementia due to Alzheimer's disease. A diagnosis of MCI offers people the chance to focus on healthy lifestyle changes and to come up with strategies to make up for memory loss. They also can schedule regular healthcare appointments to monitor symptoms.
Head injury
Several large studies found that people age 50 or older who had a traumatic brain injury, also called TBI, had a higher risk of getting dementia and Alzheimer's disease. The risk is even higher in people with serious TBIs or multiple TBIs.
Air pollution
Studies in animals have found that air pollution particulates can speed the breakdown of the nervous system. Human studies have found that air pollution exposure — especially from traffic exhaust and burning wood — is linked to a higher risk of dementia.
Heavy alcohol use
Drinking large amounts of alcohol has long been known to cause brain changes. Several large studies and reviews found that alcohol misuse is linked to a higher risk of dementia, especially early-onset dementia.
Poor sleep patterns
Research has shown that poor sleep patterns, such as trouble falling asleep or staying asleep, are linked to a raised risk of Alzheimer's disease. Sleep apnea also may raise the risk of dementia.
Lifestyle and heart health
Research has shown that the same risk factors for heart disease also may increase the risk of dementia. It's not clear if these factors raise risk by worsening Alzheimer's changes in the brain or by leading to blood vessel changes in the brain. The factors include:
- Lack of exercise.
- Obesity.
- Smoking or exposure to secondhand smoke.
- High blood pressure.
- High cholesterol.
- Poorly managed type 2 diabetes.
High levels of low-density lipoprotein, known as LDL, cholesterol in middle age, in particular, raises the risk of dementia. Research has found that people younger than 65 with high LDL cholesterol levels have a higher risk of dementia. But taking medicines to lower LDL cholesterol didn't raise the risk.
These factors can all be modified, so changing lifestyle habits can to some degree alter your risk. For example, regular exercise and a healthy low-fat diet rich in fruits and vegetables are related to a lower risk of Alzheimer's disease.
Hearing loss
Studies have found that people who have hearing loss are at risk of dementia. The worse the hearing loss, the higher the risk. However, wearing hearing aids protects against getting dementia.
Vision loss that is not treated
Newer research suggests vision loss that isn't treated is a risk factor for cognitive impairment and dementia. The link may be due to a disease such as diabetes that can increase the risk of both vision loss and dementia. But some research suggests vision loss itself may increase the risk of dementia.
Lifelong learning and social engagement
Studies have found that being social and doing activities that stimulate the mind throughout life can lower the risk of Alzheimer's disease. Low education levels — less than a high school education — appear to be a risk factor for Alzheimer's disease.
Complications
Alzheimer's disease can lead to a variety of complications. Symptoms such as memory loss, language loss, impaired judgment and other brain changes can make it harder to manage other health conditions. A person with Alzheimer's disease may not be able to:
- Tell someone about being in pain.
- Explain symptoms of another illness.
- Follow a treatment plan.
- Explain medicine side effects.
As Alzheimer's disease moves into its last stages, brain changes begin to affect physical functions. The changes can affect the ability to swallow, balance, and manage stool and bladder movements. These effects can lead to other health issues such as:
- Inhaling food or liquid into the lungs.
- Flu, pneumonia and other infections.
- Falls.
- Fractures.
- Bedsores.
- Poor nutrition or dehydration.
- Constipation or diarrhea.
Prevention
Alzheimer's disease can't be prevented. But making lifestyle changes can lower your risk of getting the disease.
Research suggests that taking steps that lower your risk of cardiovascular disease may reduce the risk of dementia, as well. To follow heart-healthy lifestyle choices that may lower the risk of dementia:
- Exercise regularly.
- Eat a diet of fresh produce, healthy oils and foods low in saturated fat, such as a Mediterranean diet.
- Work with your healthcare professional to manage high blood pressure, diabetes and high cholesterol. Pay particular attention to your levels of low-density lipoprotein, known as LDL, cholesterol. High levels of LDL cholesterol in people younger than 65 raises the risk of dementia. But taking medicines to lower LDL cholesterol doesn't raise the risk.
- If you smoke, ask your healthcare professional for help to quit.
One large, long-term study done in Finland found that making lifestyle changes helped reduce cognitive decline among people who were at risk of dementia. Those in the study were given individual and group sessions that focused on diet, exercise and social activities.
Several studies have found that following a Mediterranean diet leads to better cognitive function and a slower cognitive decline with age. A Mediterranean diet focuses on plant-based foods such as fruits, vegetables, grains, fish, poultry, nuts and olive oil. The diet includes less foods that are high in saturated fats and trans fats, such as butter, margarine, cheese, red meat, fried food and pastries.
It's also important to treat vision loss and hearing loss. Studies have found that vision loss that isn't treated is a risk factor for cognitive impairment and dementia. Studies also have found that people who have hearing loss are at higher risk of dementia. But wearing hearing aids made people less likely to get dementia.
Other studies have shown that staying engaged mentally and socially is linked to preserved thinking skills later in life and a lower risk of Alzheimer's disease. This includes going to social events, reading, dancing, playing board games, creating art, playing an instrument and other activities.
Nov. 08, 2024