Overview
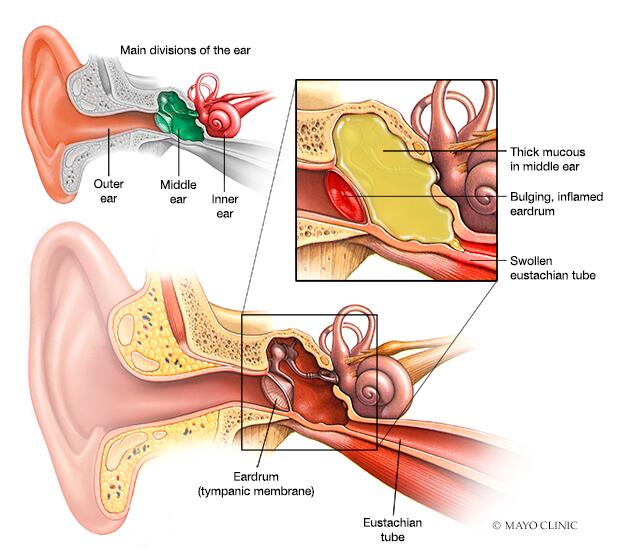
An ear infection (sometimes called acute otitis media) is an infection of the middle ear, the air-filled space behind the eardrum that contains the tiny vibrating bones of the ear. Children are more likely than adults to get ear infections.
Ear infection
In an ear infection, narrow tubes that run from the middle ear to high in the back of the throat (eustachian tubes) can become swollen and blocked. This can lead to mucus build-up in the middle ear. This mucus can become infected and cause ear infection symptoms.
Because ear infections often clear up on their own, treatment may begin with managing pain and monitoring the problem. Sometimes, antibiotics are used to clear the infection. Some people are prone to having multiple ear infections. This can cause hearing problems and other serious complications.
Symptoms
The onset of signs and symptoms of ear infection is usually rapid.
Children
Signs and symptoms common in children include:
- Ear pain, especially when lying down
- Tugging or pulling at an ear
- Trouble sleeping
- Crying more than usual
- Fussiness
- Trouble hearing or responding to sounds
- Loss of balance
- Fever of 100 F (38 C) or higher
- Drainage of fluid from the ear
- Headache
- Loss of appetite
Adults
Common signs and symptoms in adults include:
- Ear pain
- Drainage of fluid from the ear
- Trouble hearing
When to see a doctor
Signs and symptoms of an ear infection can indicate several conditions. It's important to get an accurate diagnosis and prompt treatment. Call your child's doctor if:
- Symptoms last for more than a day
- Symptoms are present in a child less than 6 months of age
- Ear pain is severe
- Your infant or toddler is sleepless or irritable after a cold or other upper respiratory infection
- You observe a discharge of fluid, pus or bloody fluid from the ear
From Mayo Clinic to your inbox
Causes
An ear infection is caused by a bacterium or virus in the middle ear. This infection often results from another illness — cold, flu or allergy — that causes congestion and swelling of the nasal passages, throat and eustachian tubes.
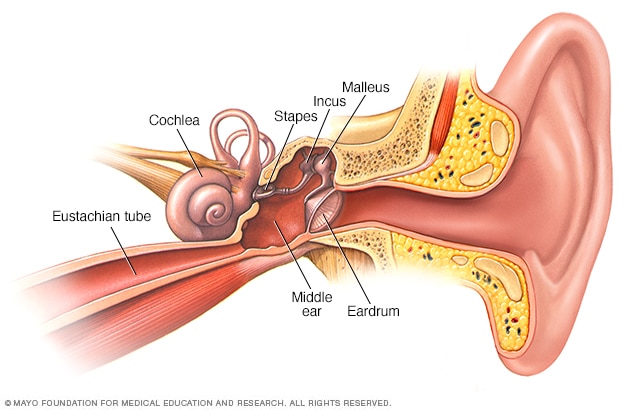
Middle ear
The middle ear has three small bones — the hammer, or malleus; the anvil, or incus; and the stirrup, or stapes. The eardrum keeps the bones away from the outer ear. A narrow path called the eustachian tube joins the middle ear to the back of the nose and upper part of the throat. The cochlea, a snail-shaped structure, is part of your inner ear.
Role of eustachian tubes
The eustachian tubes are a pair of narrow tubes that run from each middle ear to high in the back of the throat, behind the nasal passages. The throat end of the tubes open and close to:
- Regulate air pressure in the middle ear
- Refresh air in the ear
- Drain normal secretions from the middle ear
Swollen eustachian tubes can become blocked, causing fluids to build up in the middle ear. This fluid can become infected and cause the symptoms of an ear infection.
In children, the eustachian tubes are narrower and more horizontal, which makes them more difficult to drain and more likely to get clogged.
Role of adenoids
Adenoids are two small pads of tissues high in the back of the nose believed to play a role in immune system activity.
Because adenoids are near the opening of the eustachian tubes, swelling of the adenoids may block the tubes. This can lead to middle ear infection. Swelling and irritation of adenoids is more likely to play a role in ear infections in children because children have relatively larger adenoids compared to adults.
Related conditions
Conditions of the middle ear that may be related to an ear infection or result in similar middle ear problems include:
- Otitis media with effusion, or swelling and fluid buildup (effusion) in the middle ear without bacterial or viral infection. This may occur because the fluid buildup persists after an ear infection has gotten better. It may also occur because of some dysfunction or noninfectious blockage of the eustachian tubes.
- Chronic otitis media with effusion, occurs when fluid remains in the middle ear and continues to return without bacterial or viral infection. This makes children susceptible to new ear infections and may affect hearing.
- Chronic suppurative otitis media, an ear infection that doesn't go away with the usual treatments. This can lead to a hole in the eardrum.
Risk factors
Risk factors for ear infections include:
- Age. Children between the ages of 6 months and 2 years are more susceptible to ear infections because of the size and shape of their eustachian tubes and because their immune systems are still developing.
- Group child care. Children cared for in group settings are more likely to get colds and ear infections than are children who stay home. The children in group settings are exposed to more infections, such as the common cold.
- Infant feeding. Babies who drink from a bottle, especially while lying down, tend to have more ear infections than do babies who are breast-fed.
- Seasonal factors. Ear infections are most common during the fall and winter. People with seasonal allergies may have a greater risk of ear infections when pollen counts are high.
- Poor air quality. Exposure to tobacco smoke or high levels of air pollution can increase the risk of ear infections.
- Alaska Native heritage. Ear infections are more common among Alaska Natives.
- Cleft palate. Differences in the bone structure and muscles in children who have cleft palates may make it more difficult for the eustachian tube to drain.
Complications
Most ear infections don't cause long-term complications. Ear infections that happen again and again can lead to serious complications:
- Impaired hearing. Mild hearing loss that comes and goes is fairly common with an ear infection, but it usually gets better after the infection clears. Ear infections that happen again and again, or fluid in the middle ear, may lead to more-significant hearing loss. If there is some permanent damage to the eardrum or other middle ear structures, permanent hearing loss may occur.
- Speech or developmental delays. If hearing is temporarily or permanently impaired in infants and toddlers, they may experience delays in speech, social and developmental skills.
- Spread of infection. Untreated infections or infections that don't respond well to treatment can spread to nearby tissues. Infection of the mastoid, the bony protrusion behind the ear, is called mastoiditis. This infection can result in damage to the bone and the formation of pus-filled cysts. Rarely, serious middle ear infections spread to other tissues in the skull, including the brain or the membranes surrounding the brain (meningitis).
- Tearing of the eardrum. Most eardrum tears heal within 72 hours. In some cases, surgical repair is needed.
Prevention
The following tips may reduce the risk of developing ear infections:
- Prevent common colds and other illnesses. Teach your children to wash their hands frequently and thoroughly and to not share eating and drinking utensils. Teach your children to cough or sneeze into their elbow. If possible, limit the time your child spends in group child care. A child care setting with fewer children may help. Try to keep your child home from child care or school when ill.
- Avoid secondhand smoke. Make sure that no one smokes in your home. Away from home, stay in smoke-free environments.
- Breast-feed your baby. If possible, breast-feed your baby for at least six months. Breast milk contains antibodies that may offer protection from ear infections.
- If you bottle-feed, hold your baby in an upright position. Avoid propping a bottle in your baby's mouth while he or she is lying down. Don't put bottles in the crib with your baby.
- Talk to your doctor about vaccinations. Ask your doctor about what vaccinations are appropriate for your child. Seasonal flu shots, pneumococcal and other bacterial vaccines may help prevent ear infections.

