Overview
Vasectomy reversal is surgery to undo a vasectomy. During the procedure, a surgeon reconnects each tube (vas deferens) that carries sperm from a testicle into the semen. After a successful vasectomy reversal, sperm are again present in the semen, and you may be able to get your partner pregnant.
Pregnancy rates after vasectomy reversal will range from about 30% to over 90%, depending on the type of procedure. Many factors affect whether a reversal is successful in achieving pregnancy, including time since a vasectomy, partner age, surgeon experience and training, and whether you had fertility issues before your vasectomy.
Products & Services
Why it's done
Deciding to have a vasectomy reversal may happen for several reasons, including loss of a child, a change of heart or remarriage, or to treat chronic testicular pain after vasectomy.
Our caring team of Mayo Clinic experts can help you with your health concerns. Get started at Mayo Clinic Men's Health.
Get care now
Risks
Almost all vasectomies can be reversed. However, this doesn't guarantee success in conceiving a child. Vasectomy reversal can be attempted even if several years have passed since the original vasectomy — but the longer it has been, the less likely it is that the reversal will work.
Vasectomy reversal rarely leads to serious complications. Risks include:
- Bleeding within the scrotum. This can lead to a collection of blood (hematoma) that causes painful swelling. You can reduce the risk of hematoma by following your doctor's instructions to rest, use scrotal support and apply ice packs after surgery. Ask your doctor if you need to avoid aspirin or other types of blood-thinning medication before and after surgery.
- Infection at the surgery site. Although very uncommon, infections are a risk with any surgery and may require treatment with antibiotics.
- Chronic pain. Persistent pain after vasectomy reversal is uncommon.
How you prepare
When considering vasectomy reversal, here are a few things to think about:
- Vasectomy reversal may be expensive, and your insurance might not cover it. Find out about costs ahead of time.
- Vasectomy reversals are generally most successful when they're done by a surgeon who is trained in and uses microsurgical techniques, including those that make use of a surgical microscope.
- The procedure is most successful when performed by a surgeon who does the procedure regularly and who has done the procedure many times.
- The procedure occasionally requires a more complex type of repair, known as a vasoepididymostomy. Make sure that your surgeon is able to perform this procedure if it's required.
When choosing a doctor, don't be afraid to ask questions about how many vasectomy reversals the doctor has done, the type of techniques used and how often the vasectomy reversals have resulted in pregnancy. Also ask about the risks and potential complications of the procedure.
Food and medications
Make sure you know what steps you need to take before surgery. Your doctor will probably ask you to stop taking certain medications, including blood-thinning medications and pain relievers, such as aspirin or ibuprofen (Advil, Motrin IB, others), because they can increase your risk of bleeding.
Clothing and personal items
Bring tightfitting undergarments, such as an athletic supporter, to wear after surgery. This will support your scrotum and hold bandages in place.
Other precautions
Arrange for someone to drive you home after surgery. Surgery generally takes about two to four hours or longer. You may need additional time to recover if the procedure is done with general anesthesia. Ask your doctor when you can expect to go home after surgery.
What you can expect
Vasectomy reversal
Vasectomy reversal
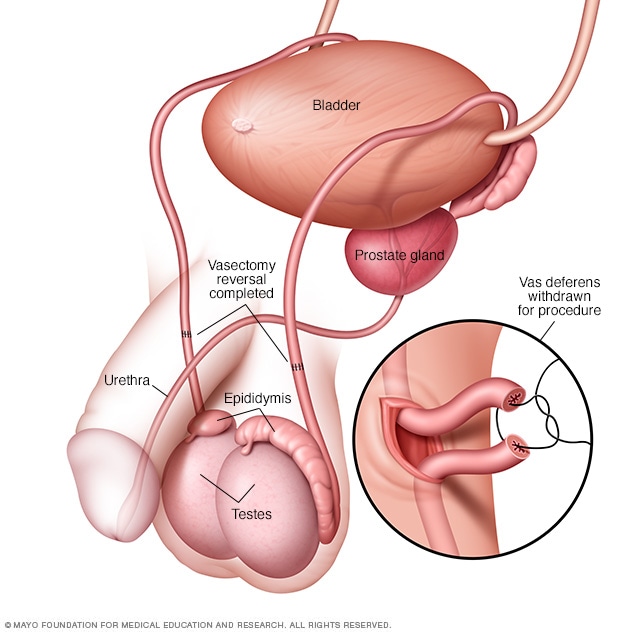
A vasectomy reversal reconnects the severed vas deferens, the tube that carries sperm from each testicle. During a vasectomy reversal, the severed ends of the vas deferens are reattached to one another. In some cases, the vas deferens may be attached directly to the epididymis — the part of the testicle where sperm matures.
Before the procedure
Before vasectomy reversal surgery, your doctor will likely want to:
- Take your history and perform a physical exam. Your doctor will want to make sure that you don't have health concerns that could complicate surgery.
- Check to see whether you can produce healthy sperm. For most men, having fathered a child before is proof enough. After your vasectomy, your testicles continued to produce sperm. But the amount of sperm that you produce may have decreased over time. Age, diet, exercise, smoking and other things can change how much healthy sperm you can produce. To be sure, your doctor may want to perform some tests before surgery.
- Confirm that your partner is capable of having a child. Your doctor will want to see whether your partner has any fertility problems, especially if your partner has never had a child or is older than age 40. This may require a gynecological exam and other tests.
Doctors usually perform vasectomy reversals at a surgery center or hospital. The procedure is generally done on an outpatient basis — without an overnight stay. Some surgeons can do the surgery in the clinic, but you'll want to make sure that the surgeon is able to do a more complex repair (vasoepididymostomy) in the clinic, if that becomes necessary.
Your doctor may use general anesthesia to make you unconscious during surgery. Or your surgeon may give you an anesthetic that keeps you from feeling pain but doesn't put you to sleep — such as a local anesthetic.
Vasectomy reversal is more difficult than a vasectomy and should be done using microsurgery, in which a surgeon uses a powerful surgical microscope to magnify the vas deferens as much as 40 times its size. This type of surgery requires specialized skills and expertise.
Doctors performing this surgery usually will reattach the vas deferens in one of two ways:
- Vasovasostomy (vas-o-vay-ZOS-tuh-me). With this procedure, the surgeon sews back together the severed ends of each tube that carries sperm (vas deferens).
- Vasoepididymostomy (vas-o-ep-ih-did-ih-MOS-tuh-me). This surgery attaches the vas deferens directly to the small organ at the back of each testicle that holds sperm (epididymis). A vasoepididymostomy is more complicated than a vasovasostomy and is generally chosen if a vasovasostomy can't be done or isn't likely to work.
The decision to perform a vasovasostomy versus a vasoepididymostomy depends on whether sperm are seen when fluid from the vas deferens is analyzed at the time of surgery.
It is not possible to know ahead of time which procedure is needed. In most cases, the surgeon decides during the operation which technique will work best. Sometimes a combination of the two surgical techniques is needed — a vasovasostomy on one side and a vasoepididymostomy on the other. The longer it has been since your vasectomy, the more likely you are to need a vasoepididymostomy on one or both sides.
Narrator: A vasovasostomy is one surgical procedure used to reverse a vasectomy. The animation provides a brief overview of the relevant anatomy with the vas deferens, prior vasectomy site, epididymis and testicle highlighted. The procedure is performed by placing the patient under anesthesia after which a midline scrotal incision is made in the scrotum. This is usually not much bigger than is required to perform the original vasectomy. The segment of vas deferens that was previously blocked or transected at the time of the initial vasectomy is identified, brought through the surgical wound and resected. After this, the fluid is sampled from the testicular end of the open vas deferens. This fluid is then analyzed under a microscope to determine if any sperm are present. In this particular case, an abundant number of motile sperm are visualized. This would suggest that we can proceed with reattachment of the vas deferens directly. To accomplish the reattachment, initial stitches are initially placed to re-approximate the vas deferens. After this step, several intraluminal smaller sutures are placed to bring the lumen of the vasa together. Additional sutures are then placed to completely enclose the opening of the vas and final supporting sutures are placed to reinforce the newly attached vas deferens. Once the sutures are tied, the final connection is complete and the vas deferens is returned to its normal location. The animation demonstrates the final result of a vasovasostomy.
Narrator: In certain conditions, a more complex reconstruction is required known as an epididymovasostomy or vasoepididymostomy. The animation provides a brief overview of the relevant anatomy with the vas deferens, prior vasectomy site, epididymis and testicle highlighted. This procedure begins in a similar manner to a vasovasostomy. A midline scrotal incision is made after which the obstructed vasal segment is removed and the fluid on the testicular side is sampled under microscopy. In this particular case, microscopic analysis does not demonstrate the presence of any sperm. In that scenario, we would proceed with an epididymovasostomy. The scrotal midline incision is extended after which the testicle is delivered through the wound. This permits better visualization of the epididymis. Next, the epididymis is incised and an obstructed epididymal tubule is selected for anastomosis. The vas deferens is brought down to the level of the epididymis and secured using some initial stitches. Two double-armed smaller sutures are then placed into the epididymal tubule after which the epididymal tubule is incised. The fluid is again sampled and this time demonstrates the presence of normal sperm. Once sperm are identified, the stitches are then placed inside the lumen of the vas deferens and the vas deferens is tied down to the epididymal tubule. Additional stitches are then placed to secure the vas deferens to the epididymal sheath for additional strength. This final animation demonstrates the post-operative result with the attachment of the vas deferens to the epididymis directly.
During the procedure
During surgery, your doctor will make a small cut (incision) on your scrotum. This will expose the tube that carries sperm (vas deferens) and release it from surrounding tissues.
Next, the doctor will cut open the vas deferens and examine the fluid inside. When sperm are present in the fluid, the ends of the vas deferens can be connected to reestablish the passageway for sperm.
If the fluid contains no sperm, scar tissue may be blocking sperm flow. In this case, your doctor may choose to perform a vasoepididymostomy.
Robot-assisted surgery has been used for vasectomy reversal but usually is required only in select cases.
After the procedure
Immediately after surgery, your doctor will cover the incision with bandages. You'll put on tightfitting undergarments, such as an athletic supporter, and apply ice for 24 to 48 hours to reduce swelling.
You may be sore for several days. If your doctor places bandages over the incision after your surgery, ask when it's OK to take them off. Any stitches should dissolve in seven to 10 days.
After you return home, take it easy and try to limit activities that might cause the testicles to move around excessively. As the anesthetic wears off, you may have some pain and swelling. For most men, the pain isn't severe and gets better after a few days to a week.
Your doctor may also give you the following instructions:
- For several weeks, wear an athletic supporter except when showering. After that, you'll need to continue to wear one when you exercise.
- For the first two days after surgery, avoid anything that might get the surgery site wet, such as bathing or swimming.
- Limit any activities that may pull on the testicles or scrotum, such as jogging, sporting activities, biking or heavy lifting, for at least six to eight weeks after surgery.
- If you have a desk job, you'll probably be able to return to work a few days after surgery. If you perform physical labor or have a job that requires much walking or driving, talk to your doctor about when it's safe to go back to work.
- Don't have sexual intercourse or ejaculate until your doctor says it's OK. Most men need to refrain from ejaculating for two to three weeks after surgery.
Freezing sperm
Although it's usually not required or recommended, you may choose to have sperm frozen (cryopreservation) in case your vasectomy reversal doesn't work. If you're not able to father a child through sexual intercourse, you may still be able to have children through assisted reproductive technology such as in vitro fertilization.
Results
Sometime after surgery, your doctor will examine your semen under a microscope to see if the operation was successful.
Your doctor may want to check your semen periodically. Unless you get your partner pregnant, checking your semen for sperm is the only way to tell if your vasectomy reversal was a success.
When a vasectomy reversal is successful, sperm may appear in the semen within a few weeks, but it can sometimes take a year or more. The likelihood of achieving pregnancy depends on various factors, including the number and quality of sperm present and the female partner's age.
If the vasectomy reversal doesn't work
Vasectomy reversals sometimes fail if there is an underlying issue with the testicle that cannot be recognized during surgery or if a blockage develops sometime after surgery. Some men have a second-attempt vasectomy reversal surgery if the procedure doesn't work the first time. Success rates are slightly lower for the second attempt than for the initial attempt.
You may also be able to father a child through in vitro fertilization by using frozen sperm. Sperm may be retrieved directly from the testicle or epididymis either at the time of the reversal surgery or at a later date. Doctors don't usually recommend freezing sperm at the time of reversal surgery, as it may be an unnecessary extra procedure.