Overview
Spinal fusion is surgery to connect two or more bones in any part of the spine. Connecting the bones prevents movement between them. Preventing movement helps prevent pain.
During spinal fusion, a surgeon places bone or a bonelike material in the space between two spinal bones. Metal plates, screws or rods might hold the bones together. The bones then can fuse and heal as one bone.
Why it's done
Spinal fusion connects two or more bones in the spine to make it more stable, correct a problem or reduce pain. Spinal fusion may help relieve symptoms caused by:
- The shape of the spine. Spinal fusion can help correct problems with the way the spine is formed. An example is when the spine curves sideways, also known as scoliosis.
- Spinal weakness or instability. Too much motion between two spinal bones can make the spine unstable. This is a common side effect of severe arthritis in the spine. Spinal fusion can make the spine more stable.
- Damaged disk. Spinal fusion might be used to stabilize the spine after a damaged disk is removed.
Risks
Spinal fusion is generally safe. But as with any surgery, spinal fusion carries some risks.
Possible complications include:
- Infection.
- Poor wound healing.
- Bleeding.
- Blood clots.
- Injury to blood vessels or nerves in and around the spine.
- Pain at the bone graft site.
- Return of symptoms.
How you prepare
Getting ready for the surgery might include trimming hair over the surgical site and cleaning the area with a special soap. Tell your healthcare team about medicines you take. You may be asked to stop taking some medicines for a time before the surgery.
What you can expect
During spinal fusion
Fusion from back of neck
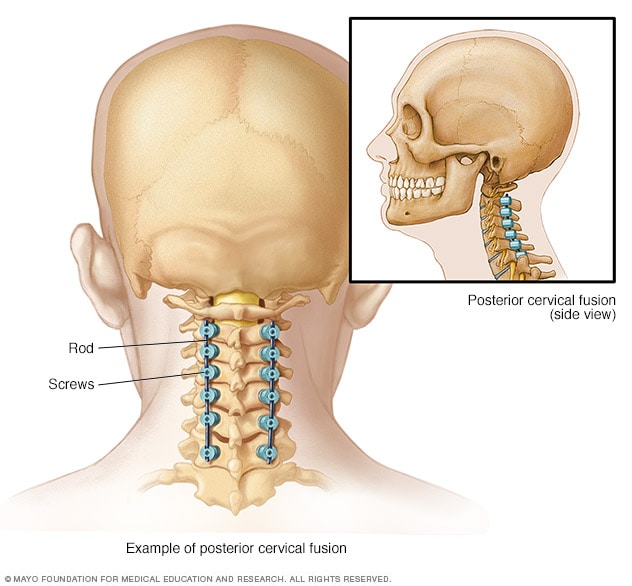
Fusion from back of neck
When spinal fusion is done from the back of the neck, this is known as posterior cervical fusion. Rods and screws are used to hold the bones together.
Fusion from front of neck
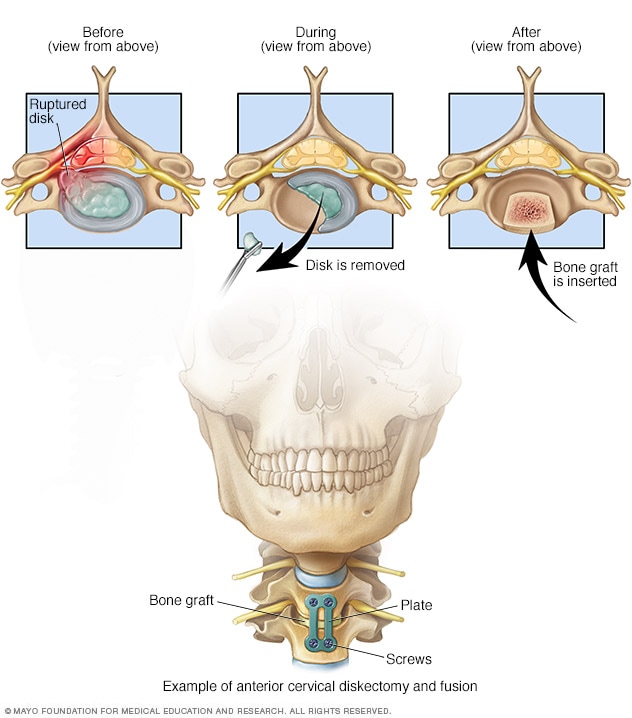
Fusion from front of neck
Sometimes, surgery on the spinal bones of the neck occurs from the front. In the example shown, a damaged disk is removed, a bone graft is inserted, and plates and screws hold the bones together. This procedure is called anterior diskectomy and fusion.
Fusion options for lower back
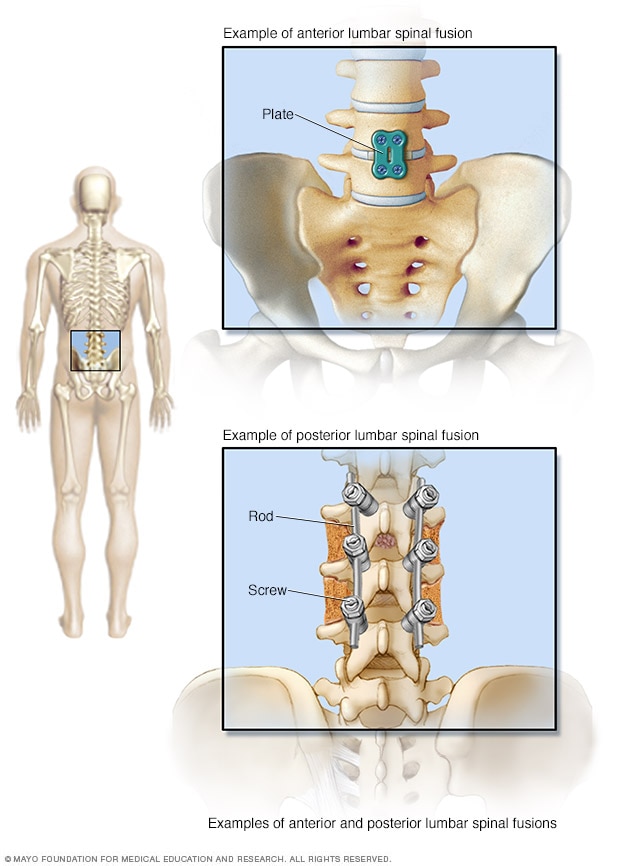
Fusion options for lower back
A surgeon can get to the spine from the front, known as an anterior spinal fusion. From the back, it's known as posterior spinal fusion. With either entry point, a metal plate or rods and screws are inserted to hold the bones together until the bones heal.
Surgeons perform spinal fusion while the person having the procedure is in a deep sleeplike state, known as general anesthesia. There are several ways to do spinal fusion surgery. The technique the surgeon uses depends on where the bones to be fused are on the spine, the reason for the spinal fusion, and possibly, general health and body shape.
Generally, the procedure involves the following:
- Getting to the spine. To get to the bones being fused, the surgeon cuts in one of three places. From the back, these cuts are in the neck or back directly over the spine or on either side of the spine. To get to the spine from the front, the surgeon cuts into the stomach area or throat.
- Getting the bone graft ready. Bone grafts come from a bone bank or from the body of the person having the surgery, usually from the pelvis. Sometimes surgeons use human-made material instead of bone grafts. To use the person's bone, the surgeon cuts near the pelvic bone, removes a small part of it and then closes the cut.
- Fusion. To fuse the spinal bones, the surgeon places the bone graft material between the bones. The surgeon might use metal plates, screws or rods to help hold the bones together while the bone graft heals.
After spinal fusion
A hospital stay of 2 to 3 days is usually required following spinal fusion. Depending on the location and extent of your surgery, you may experience some pain and discomfort. Medicines usually can control pain.
At home after surgery, contact your healthcare team if there are signs of infection. Watch for:
- A change in color around the wound. This might be a shade of red, purple or brown depending on your skin color.
- Tenderness or swelling in the wound area.
- Fluid coming from the wound.
- Chills that cause shaking.
- Fever higher than 100.4 degrees Fahrenheit (38 degrees Celsius).
It can take several months for the bones in the spine to heal and fuse. A healthcare professional might suggest wearing a brace for a time to keep the spine straight. Physical therapy can teach how to move, sit, stand and walk in a way that keeps the spine in line.
Results
Spinal fusion typically works for fixing broken bones, reshaping the spine or making the spine more stable. But study results are mixed when the cause of the back or neck pain is not clear. Spinal fusion often works no better than nonsurgical treatments for back pain with a cause that's not clear.
Even when spinal fusion relieves symptoms, it doesn't prevent future back pain. Arthritis causes much of back pain. Surgery doesn't cure arthritis.
Having a spine that doesn't move in places puts more strain on the areas around the fused part. As a result, those areas of the spine might break down faster. Then the spine might need more surgery in the future.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Nov. 26, 2024