Overview
Pap test
Pap test
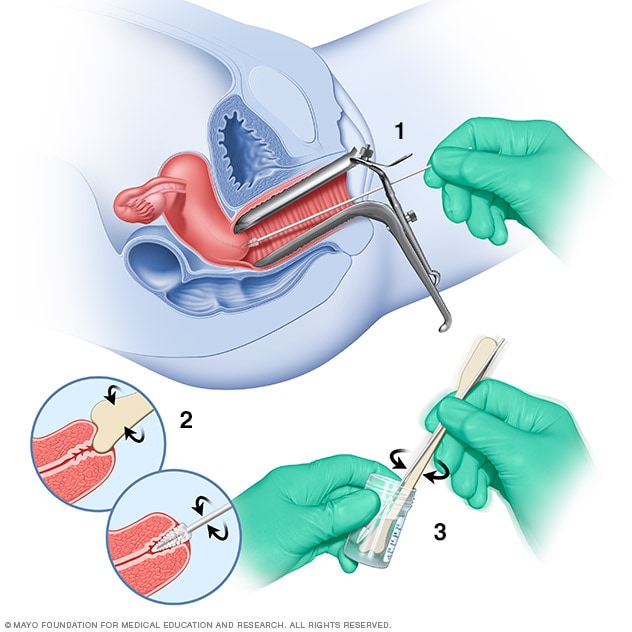
During a Pap test, a tool called a speculum holds the vaginal walls apart. A sample of cells from the cervix is collected using a soft brush and a flat scraping device called a spatula (1 and 2). The cells are placed in a bottle that contains a solution to preserve them (3). Later, the cells are checked under a microscope.
A Pap smear is a procedure that involves collecting cells from the cervix for testing. It also is called a Pap test. Healthcare professionals sometimes call it cervical cytology.
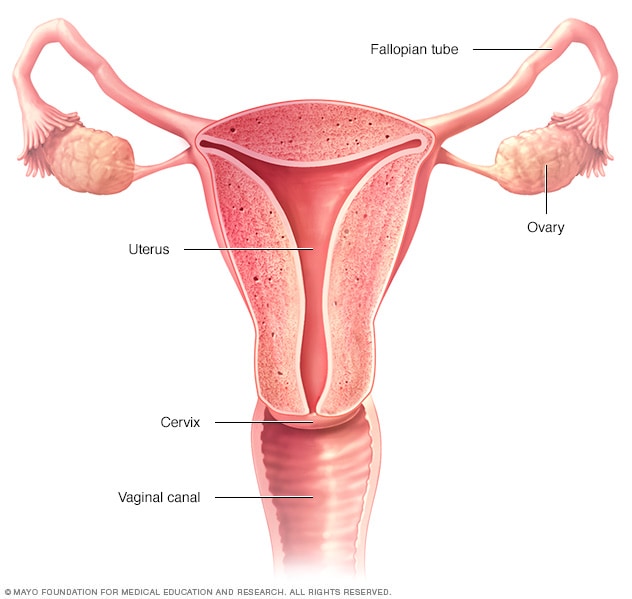
A Pap test is often used to look for cervical cancer. Cervical cancer is cancer that starts as a growth of cells in the cervix. The cervix is the lower, narrow end of the uterus that opens into the vagina. Cervical cancer screening with a Pap test can find cervical cancer early, when it's more likely to be cured.
In addition to looking for cancer cells, a Pap test also looks for cells that could become cancer in the future. If the test finds precancerous cells, treatments could help prevent cancer.
Products & Services
Why it's done
A Pap smear looks for cervical cancer. It's one option for cervical cancer screening in anyone who has a cervix. A Pap smear also is called a Pap test.
The Pap test usually is done at the same time as a pelvic exam. During a pelvic exam, a healthcare professional checks the reproductive organs. Sometimes the Pap test may be combined with a test for human papillomavirus, also called HPV. HPV is a common virus that's passed through sexual contact. Most cervical cancers are caused by HPV. Sometimes the HPV test is used instead of a Pap test for cervical cancer screening.
You and your healthcare professional can decide when it's time for you to begin cervical cancer screening and how often it should be repeated.
Recommendations for cervical cancer screening may depend on your age:
- In your 20s: Get your first Pap test at age 21. Repeat the test every three years. Sometimes the Pap test and HPV test are done at the same time. This is called co-testing. Co-testing may be an option starting at age 25. Co-testing is typically repeated every five years.
- After age 30: Cervical cancer screening after 30 often involves co-testing with a Pap test and HPV test every five years. Sometimes the HPV test is used alone and repeated every five years.
- After age 65: Consider stopping cervical cancer screening after discussing your health history and risk factors with your healthcare professional. If your cervical cancer screening tests haven't found anything that's not typical, you may choose to stop the screening tests.
Cervical cancer screening might not be needed after total hysterectomy. Total hysterectomy is surgery to remove the uterus and cervix. If your hysterectomy was done for a reason other than cancer, you might consider stopping Pap tests. Talk with your healthcare professional about what's best in your situation.
If you have certain risk factors, your healthcare professional may recommend Pap tests more often. These risk factors include:
- A diagnosis of cervical cancer.
- A Pap test that showed precancerous cells.
- Exposure to diethylstilbestrol, also called DES, before birth.
- HIV infection.
- Weakened immune system.
You and your healthcare professional can discuss the benefits and risks of Pap tests and decide what's best for you.
More Information
Risks
A Pap smear is a safe way to screen for cervical cancer. Still, a Pap smear, also called a Pap test, isn't always accurate. It's possible to receive a false-negative result. This means that cancer cells or other concerning cells are present, but the test doesn't find them.
A false-negative result doesn't mean that a mistake was made. A false-negative result could happen because:
- Too few cells were collected.
- Too few concerning cells were collected.
- Blood or infection may hide cells that are concerning.
- Douching or vaginal medicines may have washed away the concerning cells.
Cervical cancer takes many years to develop. If one test doesn't find the concerning cells, the next test probably will. That is why healthcare professionals recommend having regular Pap tests.
How you prepare
To ensure that your Pap smear is most effective, follow your healthcare professional's instructions about how to prepare. Before a Pap smear, also called a Pap test, you may be asked to:
- Avoid intercourse, douching, or using any vaginal medicines or spermicidal foams, creams or jellies for two days before having a Pap test. These may wash away or hide concerning cells.
- Try not to schedule a Pap test during your menstrual period. While it can be done at this time, it is best not to do so. If you have bleeding that is not part of your regular period, do not delay your test.
What you can expect
During the test
Female reproductive system
Female reproductive system
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
A Pap smear is performed in a healthcare professional's office. A Pap smear, also called a Pap test, typically takes only a few minutes. You may be asked to undress completely or only from the waist down.
You'll lie down on your back on an exam table with your knees bent. Your heels rest in footrests called stirrups.
Your healthcare professional will gently put an instrument called a speculum into your vagina. The speculum holds the walls of your vagina apart so that your cervix is easily seen. The speculum may cause a feeling of cramping or pressure.
Then, your healthcare professional will take samples of your cervical cells using a soft brush and a small stick called a spatula. This usually doesn't hurt. You may have some light bleeding from the vagina afterward.
The healthcare professional places your collected cervix cells into a special liquid. The liquid goes to a lab. In the lab, the cells are examined under a microscope to look for signs of cancer or concerning cells that could become cancer.
After the test
After your Pap test, you can go about your day as usual.
Ask your healthcare professional when you can expect the results of your test.
Results
Pap smear results may be ready in 1 to 3 weeks. Ask your healthcare professional when you can expect the results of your Pap smear, which is also called a Pap test.
Negative results
If your Pap test showed only healthy cervical cells, it is called a negative result. Sometimes the results will say the cells found were normal. You won't need any more treatment or testing until you're due for your next Pap test and pelvic exam.
Results that were not clear
Sometimes the results aren't clear. You may need more testing. Or your healthcare professional may ask you to return later for another Pap test.
Positive results
If concerning cells were found in your Pap smear, it is called a positive result. A positive result doesn't mean that you have cervical cancer. A positive result can mean different things depending on the type of cells found. You likely will need follow-up testing.
Here are some terms your healthcare professional might use and possible next steps:
-
Atypical squamous cells of undetermined significance, also called ASC-US. Squamous cells are thin and flat and grow on the surface of a healthy cervix. This result means that the Pap test found squamous cells that look different than healthy cells. But the cells don't look like precancerous cells. These cells are often a sign of HPV infection.
Your healthcare professional will likely have your cervical cells tested for HPV. If no high-risk viruses are present, the atypical cells aren't of great concern. If worrisome viruses are present, you may need further testing.
Squamous intraepithelial lesion, also called SIL. This result means that the cells collected from the Pap test may be precancerous. The cells can be low grade or high grade.
If the cells are low grade, this is usually caused by an HPV infection that often goes away on its own. If the cells are high grade, there's a greater chance that they may be precancerous or cancer. More testing may be needed.
- Atypical glandular cells. Glandular cells are another type of cell found in the cervix. This result means glandular cells that look different from healthy glandular cells were found. It may not be clear if the cells are cancerous. Further testing will be needed to find out if the cause of the atypical glandular cells is concerning.
- Squamous cell cancer or adenocarcinoma cells. This result means the cells collected for the Pap test are almost certainly cancer. Squamous cell cancer is cancer that starts in the flat cells on the surface of the vagina or cervix. Adenocarcinoma arises in glandular cells. If either of these cells are found, your healthcare professional will recommend prompt further testing.
If your Pap test results are concerning, your healthcare professional will perform a procedure called colposcopy. Colposcopy is an exam that looks closely at the cervix. It uses a special magnify instrument to do this.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.