Overview
Sigmoidoscopy exam
Sigmoidoscopy exam
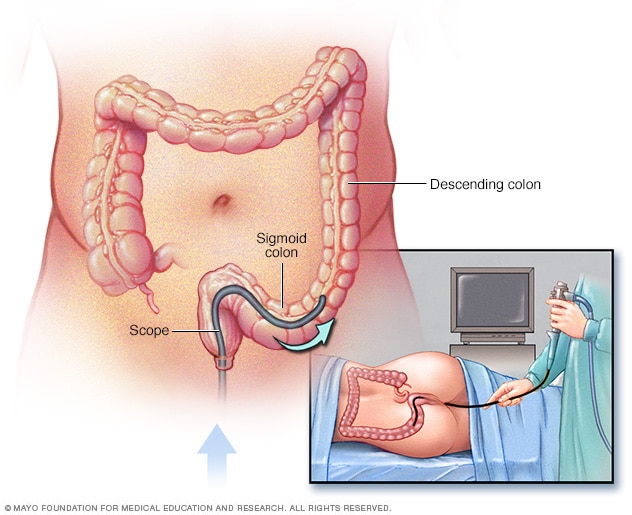
During a flexible sigmoidoscopy exam, the healthcare professional puts a sigmoidoscope into the rectum to check the lower colon.
A flexible sigmoidoscopy is an exam to see inside the rectum and part of the large intestine. A flexible sigmoidoscopy (sig-moi-DOS-kuh-pee) exam is performed using a thin, flexible tube with a light, camera and other tools, called a sigmoidoscope.
The large intestine is called the colon. The last section of the colon that connects to the rectum is called the sigmoid colon.
During a sigmoidoscopy, the examiner inserts the tube into the anus and guides it through the rectum, sigmoid colon and most of the descending colon on the left side of the body. It doesn't pass through the entire colon.
The camera allows the healthcare professional to see irregular tissues. These may include cancer or small growths, called polyps, that can develop into cancer. Polyps or small tissue samples can be removed with special sigmoidoscope tools.
If cancer or polyps are found, it's likely there will be problems throughout the colon. You may need a follow-up exam with a similar procedure, called a colonoscopy (koe-lun-OS-kuh-pee), for viewing the entire colon.
Why it's done
Your healthcare professional may use a flexible sigmoidoscopy exam to find the cause of:
- Belly pain that doesn't go away.
- Bleeding from the rectum.
- Changes in stool habits.
- Weight loss that isn't intended.
Cancer screening
Sigmoidoscopy is used to screen for colon cancer or polyps that can lead to cancer. The U.S. Preventive Services Task Force recommends a first screening at age 45. People with a higher risk of colon cancer may have a first test at age 40. After age 75, your healthcare professional and you can consider how often you have the test based on your overall health, the results of previous tests and your preferences.
Colon cancer screening with sigmoidoscopy is recommended every five years until age 75. If you have an annual stool test, called a fecal immunochemical test (FIT), the time between sigmoidoscopies may be longer.
A complete colonoscopy is also a screening tool for colon cancer. It's recommended every 10 years.
Compared with a colonoscopy, a sigmoidoscopy:
- Takes less time for you to prepare.
- Takes less time for the healthcare professional to do.
- Usually doesn't require anesthesia to put a person to sleep.
- Has a lower risk of damage to the rectum and colon.
More Information
Risks
A flexible sigmoidoscopy poses few risks. Rarely, complications of a flexible sigmoidoscopy may include:
- Bleeding from the site where a tissue sample was taken.
- A tear in the wall of the rectum or colon called a perforation.
How you prepare
Make plans for someone to drive you home after the procedure.
Before a flexible sigmoidoscopy, you'll need to empty your colon. This preparation allows the lining of the colon to be seen clearly.
To empty your colon, follow instructions carefully. You may be asked to do the following:
- Follow a special diet the day before the exam. You may be asked not to eat or drink anything after midnight the night before the exam. Your options will likely include:
- Fat-free broth.
- Plain water.
- Light-colored filtered juices, such as apple or white grape.
- Lemon, lime or orange sports drinks.
- Lemon, lime or orange gelatins.
- Tea and coffee without milk or cream.
-
Use a bowel prep kit. Your healthcare professional will tell you what kind of bowel prep kit to use. These kits have medicines to clear stool from your colon. You will frequently pass stools, so you will need to be near the toilet.
Follow the instructions on the packaging. Take doses at the time indicated in the instructions. A prep kit may have some combination of:
- Laxatives taken as pills or liquids that loosen stool.
- Enemas that are released into the rectum to clear it of stool.
- Adjust your medicines. At least a week before the exam, talk to your healthcare professional about any medicines, vitamins or supplements you take. This is especially important if you have diabetes, if you take medicines or supplements that contain iron, or if you take aspirin or other blood thinners. You may need to adjust your dosages or stop taking the medicines temporarily.
What you can expect
During the exam
Anesthesia and pain medicines usually aren't necessary. Your healthcare professional may give you medicine that helps you relax or makes you sleepy.
You will wear a hospital gown. You'll lie on your left side on the exam table, usually with your knees drawn toward your chest. The healthcare professional will insert the sigmoidoscope into your anus and direct it through your rectum and into the sigmoid colon.
The sigmoidoscope tube allows the healthcare professional to place air with carbon dioxide into your colon. This expands the colon to provide a better view of the colon lining. When the scope is moved further into the colon, you may feel cramping or the urge to move your bowels.
The sigmoidoscope also contains a tiny video camera at its tip. The camera sends live images of the colon to a screen like a computer monitor. Instruments also can pass through the scope for taking tissue samples.
A flexible sigmoidoscopy typically takes about 15 to 20 minutes. It may require slightly more time if biopsies are taken.
After the exam
After the exam, you may have mild discomfort around your belly. You may feel bloated or pass gas for a few hours. Walking may help relieve any discomfort.
You should be able to return to your usual diet and activities right away. If you had medicine to help you relax or feel sleepy, you won't be able to drive right away.
If polyps were removed or tissue samples were taken, you may notice a small amount of blood with your first bowel movement after the exam.
Call your healthcare professional if you have:
- Bloody stools or blood clots.
- Bleeding from the rectum.
- Belly pain that's severe or doesn't go away.
- Fever of 100 Fahrenheit (37.8 Celsius) or higher.
Results
Some results of a sigmoidoscopy can be shared right after the test. Some results may require lab studies. Your healthcare professional can explain whether the results were negative or positive.
- A negative result means your exam found no irregular tissues.
- A positive result means that your healthcare professional found polyps, cancer or other diseased tissue.
If polyps or biopsies were taken, they will be sent to a lab to be examined by a specialist. Also, if a sigmoidoscopy shows polyps or cancer, you'll likely need a colonoscopy to find or remove other tissues in the entire colon.
If the quality of the video imaging was poor because of unsuccessful bowel prep, your healthcare professional may schedule a repeat test or other screening or diagnostic tests.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.