Overview
Pancreatic ultrasound
Pancreatic ultrasound
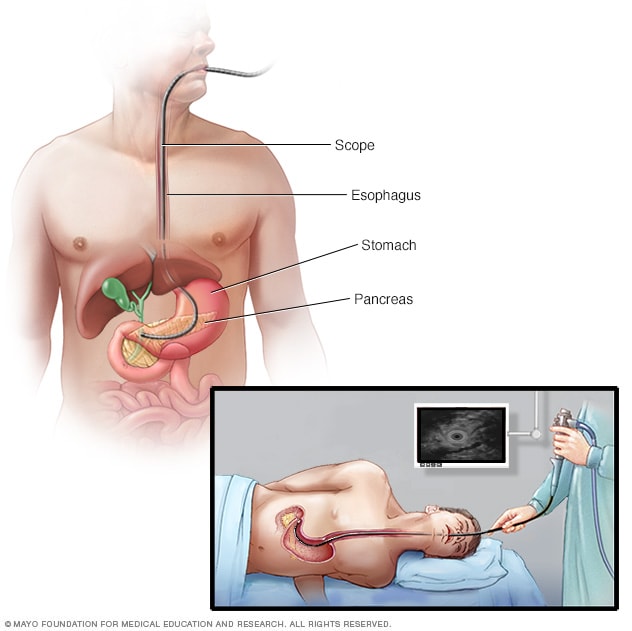
During an endoscopic ultrasound of the pancreas, a thin, flexible tube called an endoscope is inserted down the throat and into the chest. An ultrasound device at the end of the tube emits sound waves that generate images of the digestive tract and nearby organs and tissues.
Endoscopic ultrasound is a procedure that combines endoscopy and ultrasound to create images of the digestive tract and nearby organs and tissues. It also is called EUS. During EUS, a thin, flexible tube called an endoscope is placed in the digestive tract. An ultrasound device on the tip of the tube uses high-frequency sound waves to create detailed images of the digestive tract and other organs and tissues. These include the lungs, pancreas, gall bladder, liver and lymph nodes. EUS helps find diseases in these organs and tissues and the digestive tract.
Sometimes a small needle is attached to the tube. This device is used to remove fluid or tissue that will be tested in a lab. This type of sample is called a biopsy. This procedure is called EUS-guided fine-needle aspiration or EUS-guided fine-needle biopsy. EUS also can be used to drain fluid from a lesion or deliver medicine to a specific place in the body.
Products & Services
Why it's done
EUS helps diagnose conditions that affect the digestive tract and nearby organs and tissues. An EUS tube placed down the throat captures images of the esophagus, stomach and parts of the small intestine. Sometimes an EUS tube is placed through the anus, which is the muscular opening at the end of the digestive tract where stool exits the body. During this procedure, EUS captures images of the rectum and parts of the large intestine, which is called the colon.
EUS can capture images of other organs and nearby tissues too. They include:
- Lungs.
- Lymph nodes in the center of the chest.
- Liver.
- Gall bladder.
- Bile ducts.
- Pancreas.
Sometimes, needles are used as part of EUS-guided procedures to check or treat organs near the digestive tract. For example, a needle can pass through the wall of the esophagus to nearby lymph nodes. Or a needle can pass through the wall of the stomach to deliver medicine to the pancreas.
EUS and EUS-guided procedures may be used to:
- Check damage to tissues due to swelling or disease.
- Find out if cancer is present or has spread to lymph nodes.
- See how much a cancerous tumor has spread to other tissues. A cancerous tumor also is called a malignant tumor.
- Identify the stage of the cancer.
- Provide more-detailed information about lesions found by other imaging technologies.
- Take out fluid or tissue for testing.
- Drain fluids from cysts.
- Deliver medicine to a targeted region, such as a cancerous tumor.
More Information
Risks
EUS is generally safe when done at a center with an experienced healthcare team. The procedure is usually done by a doctor who specializes in the digestive system and has specific training doing EUS procedures. This doctor is called a gastroenterologist.
Your healthcare team will talk to you about the risk of complications with EUS. The risks are often related to fine-needle aspiration and may include:
- Bleeding.
- Infection.
- Tearing of an organ wall, also called a perforation.
- Pancreatitis, which sometimes happens with fine-needle aspiration of the pancreas.
To lower your risk of complications, be sure to follow instructions from your healthcare team when preparing for EUS.
Call a member of your healthcare team right away or go to an emergency room if you develop any of these symptoms after the procedure:
- Fever.
- Severe or constant stomach pain.
- Neck or chest pain.
- Severe nausea or vomiting.
- Vomiting blood.
- Black or very dark-colored stool.
How you prepare
Your healthcare team will tell you how to get ready for your EUS. Instructions include:
- Fasting. You may be asked to have nothing to eat or drink for at least six hours before the procedure to make sure your stomach is empty.
- Colon cleansing. You'll need to clean out your colon for EUS that will be done through the anus. You may be asked to use a colon cleansing solution or follow a liquid diet and use a laxative.
- Medicines. Your healthcare team may tell you to stop taking some of your medicines before EUS. Tell your healthcare team about all prescription and nonprescription medicines you take. Be sure to mention any herbal remedies and dietary supplements that you use.
- Getting home. Medicines that help you relax or sleep during EUS may make your movements a little clumsy or make it hard to think clearly after the procedure. Have someone drive you home and stay with you the rest of the day.
What you can expect
If you're given anesthesia, you won't be awake during the procedure. If you're given a sedative, you may feel some discomfort. But many people fall asleep or are not fully alert during EUS.
You'll probably lie on your left side during the procedure. The doctor feeds a thin, flexible tube through your throat or your anus, depending on what organs or tissues need to be checked.
The end of the tube has a tiny ultrasound device. This device uses sound waves to create images. Other instruments used during the procedure also pass through a channel in the tube. These instruments include a needle used to take tissue samples.
EUS usually lasts less than an hour. An EUS-guided procedure may last longer.
You may have a sore throat after an upper EUS procedure. Throat lozenges may help your throat feel better.
Results
A doctor with special training in EUS will look at the images. This may be a gastroenterologist or a pulmonologist. A pulmonologist is a doctor who treats lung disease. If you have fine-needle aspiration, a doctor trained in studying biopsies will look at the test results. This doctor is a pathologist. Your healthcare team will go over the findings and next steps with you.
Sept. 10, 2024