Overview
Intraoperative MRI
Intraoperative MRI
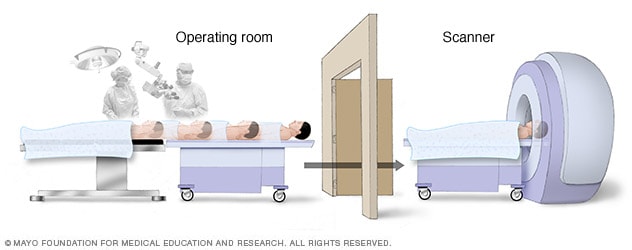
Since the brain can shift during surgery, brain-mapping techniques and intraoperative MRI create accurate pictures of the brain. These images guide the neurosurgeon to remove only the tissue that needs to be removed and focus on the targeted region for therapy. This allows the neurosurgeon to leave functional brain tissue untouched. Doing so helps preserve motor function, language and other important brain functions.
In computer-assisted brain surgery, surgeons use imaging technologies to create a 3D model of the brain. The imaging may include magnetic resonance imaging (MRI), intraoperative MRI, computerized tomography (CT) and positron emission tomography (PET) scans. Specialized fusion software allows multiple types of imaging to be used. The imaging may be done before surgery and is sometimes done during surgery.
This model allows the brain surgeon, known as a neurosurgeon, to plan the safest way to treat the condition needing surgery. During the surgery, the computer system precisely guides the surgeon to the area of the brain being treated.
Why it's done
Deep brain stimulation
Deep brain stimulation
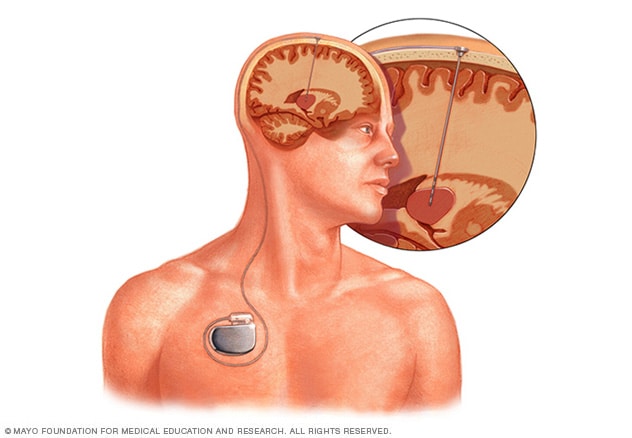
Deep brain stimulation involves putting electrodes deep within the brain. The impulses from the electrodes help the body manage the brain activity that causes seizures. The electrodes attach to a pacemakerlike device placed under the skin of the chest. The device manages how much stimulation happens.
Computer-assisted brain surgery is used to treat a variety of conditions affecting the brain. Conditions include brain tumors, Parkinson's disease, essential tremor, epilepsy and arteriovenous malformations.
If you have a brain tumor, your surgeon may combine computer-assisted surgery with awake brain surgery.
Neurosurgeons also use computer-assisted techniques when using precisely focused beams of radiation, known as stereotactic radiosurgery. Stereotactic radiosurgery may be used to treat brain tumors, arteriovenous malformations, trigeminal neuralgia and other conditions.
Computer-assisted surgery may be used when implanting electrodes for deep brain stimulation or responsive neurostimulation. Your surgeons may use MRI or CT scans — or sometimes both — to help map your brain and plot the placement of the electrodes. This may be done if you have essential tremor, Parkinson's disease, epilepsy, dystonia or obsessive-compulsive disorder.
Risks
Computer-assisted brain surgery helps to lower the risks of surgeries. By creating a 3D model of your brain, your neurosurgeon can plan the safest way to treat your condition. Computer assistance also helps guide your surgeon to the precise areas of the brain that need treatment. However, every surgery carries some risk.
Stereotactic radiosurgery has few risks, and potential side effects are often temporary. They may include feeling very tired, and soreness and swelling at the treatment site. Side effects also may include scalp irritation. Rarely, brain changes may occur months after the surgery.
Deep brain stimulation also has risks, including infection, bleeding, seizures and stroke.
If part of the skull is removed for surgery, potential risks include bleeding, swelling or infection.
How you prepare
Follow the instructions from your healthcare team about what to do in the days and hours before brain surgery. You may need to stop certain medicines before surgery.
For example, blood-thinning medicines slow the blood-clotting process. These medicines can increase the risk of bleeding. Talk to your healthcare team about whether you need to stop taking a blood-thinning medicine before surgery and for how long.
What you can expect
What happens during computer-assisted brain surgery depends on the type of surgery you're having. A medicine that puts you in a sleep-like state, known as general anesthesia, often is used in computer-assisted brain surgery. If you're having awake brain surgery, you're given medicines to feel relaxed and block pain but that keep you awake. This allows you to interact with the surgery team to maximize safety during surgery.
Sometimes a piece of skull is removed to operate on the brain. In other surgeries, such as stereotactic radiosurgery, no cuts are made. Instead, radiation is aimed at the area of the brain needing treatment.
Your neurosurgeon may take imaging scans during surgery, known as intraoperative MRI or CT using a portable CT scanner. The imaging machine used to take the images may be in the operating room and brought to you for the imaging. Or it may be in a room next door and you're brought to the machine for the images.
Results
Computer-assisted brain surgery helps surgeons more precisely plan and conduct brain surgeries. When brain surgery is more precise, it leads to better outcomes and fewer complications.
Using imaging during surgery, known as intraoperative MRI or CT, helps neurosurgeons take into account changes to the brain that occur during surgery. For example, the brain can shift during surgery. Taking images during surgery helps to make the surgery more precise. Intraoperative imaging also alerts surgeons to complications so that they can be addressed quickly.
Some research has found that using intraoperative MRIs helps surgeons more completely remove a tumor or damaged tissue. Computer-assisted brain surgery also allows more healthy tissue to be spared while targeting only the brain tissue that's being operated on.