Overview
Cardioversion
Cardioversion
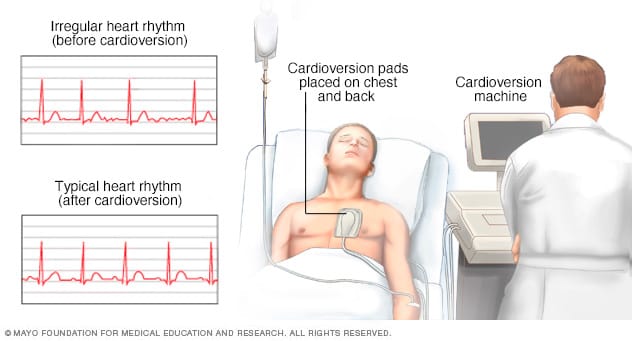
During cardioversion, a machine is used to deliver low-energy shocks to the chest while a healthcare professional watches the heart rhythm.
Cardioversion is a medical treatment that uses quick, low-energy shocks to restore a regular heart rhythm. It's used to treat some types of irregular heartbeats, called arrhythmias. An example is atrial fibrillation (AFib). Sometimes cardioversion is done using medicines.
Cardioversion is usually a scheduled appointment but is sometimes done as an emergency treatment. Usually, cardioversion quickly resets the heart rhythm.
Cardioversion is not the same as defibrillation. That's an emergency procedure that's done when the heart stops or quivers uselessly.
Products & Services
Why it's done
Cardioversion is done to correct a heartbeat that's too fast or irregular.
You may need this treatment if you have a heart rhythm disorder such as:
- Atrial fibrillation (AFib).
- Atrial flutter.
There are two main types of cardioversion.
- Electric cardioversion uses a machine and sensors to deliver quick, low-energy shocks to the chest. This type lets a healthcare professional instantly see if the treatment has corrected the irregular heartbeat.
- Chemical cardioversion, also called pharmacological cardioversion, uses medicine to reset the heart rhythm. It takes longer to work than electric cardioversion. No shocks are given during this type of cardioversion.
Risks
Cardioversion risks are uncommon. Your healthcare team can take steps to lower your risk.
Possible risks of electric cardioversion include:
-
Complications from blood clots. Some people who have irregular heartbeats, such as AFib, have blood clots form in the heart. Shocking the heart can cause these blood clots to move to other parts of the body such as the lungs or brain. This can cause a stroke or pulmonary embolism.
Tests are usually done before cardioversion to check for blood clots. Some people may be given blood thinners before the treatment.
- Other irregular heartbeats. Rarely, some people get other irregular heartbeats during or after cardioversion. These new irregular heartbeats usually happen minutes after the treatment. Medicines or additional shocks can be given to correct the heart rhythm.
- Skin burns. Rarely, some people get minor burns on their skin from the sensors placed on the chest during the test.
Cardioversion can be done during pregnancy. But it's recommended that the baby's heartbeat also be watched during the treatment.
How you prepare
Cardioversion is usually scheduled in advance. If irregular heartbeat symptoms are severe, cardioversion may be done in an emergency setting.
Before cardioversion, you may have an ultrasound of the heart called an echocardiogram to check for blood clots in the heart. Cardioversion can make blood clots move, causing life-threatening complications. Your healthcare professional tells you whether you need this test before cardioversion.
If you have one or more blood clots in the heart, cardioversion is usually delayed for 3 to 4 weeks. During that time, you usually take blood thinners to lower the risk of complications.
What you can expect
Before the procedure
You typically can't eat or drink anything for about eight hours before cardioversion.
Your healthcare team tells you whether to take any of your regular medicines before your treatment.
During the procedure
Cardioversion is usually done in the hospital. A healthcare professional puts an IV into your forearm or hand. You get medicine called a sedative to help you feel calm or less anxious during the treatment.
If you're having chemical cardioversion, you get medicine through the IV that resets the heart rhythm.
If you're having electric cardioversion, a health professional places several large patches with sensors on them on your chest and sometimes your back. Wires connect the sensors to a machine. The machine records your heart rhythm. It then delivers quick, low-energy shocks to the heart to treat the irregular heartbeats. Electric cardioversion usually takes only a few minutes to complete.
After the procedure
You usually spend an hour or so in a recovery room. A healthcare professional closely watches you for any complications.
If electric cardioversion was a scheduled procedure, you can usually go home the same day. You need someone to drive you home.
After cardioversion, you get blood-thinning medicines to prevent blood clots. You typically take these medicines for several weeks. You need blood thinners even if no clots were found in your heart before the treatment.
Results
Your healthcare professional talks with you about the treatment results. Usually, cardioversion quickly restores a regular heart rhythm. But some people need more treatments to keep the regular rhythm.
Your care team may ask you to make lifestyle changes to improve your heart health. Healthy lifestyle habits can prevent or treat conditions, such as high blood pressure, that can cause irregular heartbeats.
Try these heart-healthy tips:
- Do not smoke or use tobacco.
- Eat a healthy diet. Choose fruits, vegetables and whole grains. Limit salt, sugar, and saturated and trans fats.
- Get regular exercise. Ask your healthcare professional what a safe amount is for you.
- Keep a healthy weight.
- Get 7 to 8 hours of sleep daily.
- Take steps to reduce emotional stress.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.