Risks
Breast reconstruction with flap surgery carries a risk of complications. Complications may be related to the surgery or to the tissue flaps.
Risks of surgery
The risks of breast reconstruction surgery include:
- Slow healing of cuts in the skin, called incisions.
- Infection.
- Bleeding.
- Risks linked to the medicine that puts you in a sleeplike state during surgery. The medicine is called a general anesthetic. Risks include nausea, vomiting and confusion.
Risks of having flap surgery
The risks of having breast reconstruction with tissue flaps include:
- Tissue death, called necrosis, from too little blood supply to the new breast.
- Loss of feeling at the place where the tissue flap is taken from.
- A weakness in the belly wall that may let tissue come through, making a bulge. This is called an abdominal hernia.
Radiation therapy to the skin and chest wall after breast reconstruction with flap surgery may cause complications during healing. Your healthcare team may suggest that you wait until after radiation therapy to have breast reconstruction with flap surgery.
How you prepare
If you're thinking about breast reconstruction with flap surgery, talk with a plastic surgeon about your options. Choose a plastic surgeon who is board certified and experienced in breast reconstruction after mastectomy. It's ideal if your breast cancer surgeon and the plastic surgeon work together. Then they can come up with the best surgical treatment and breast reconstruction plan for you.
Your plastic surgeon talks with you about your surgical choices and the pros and cons of reconstruction with flap surgery. You may see photos of people who have had different types of breast reconstruction.
Your body type, health and cancer treatment go into deciding which type of reconstruction will give you the best result. The plastic surgeon talks with you about where the surgery will take place and what follow-up procedures you might need.
Some people choose to have surgery on the other breast so that it matches the new breast. Ask your plastic surgeon about the pros and cons of having surgery on your other breast.
Your healthcare team may provide instructions about how to get ready for surgery. The instructions might include stopping or changing some medicines. The instructions also might say to quit smoking if you smoke. Smoking makes it harder for the body to heal after surgery. Follow your healthcare team's instructions carefully.
What you can expect
What you can expect depends on how you and your surgery team decide to do your reconstruction. Breast reconstruction with flap surgery often starts right after mastectomy surgery. Some people choose to wait to have reconstruction surgery after they've healed from a mastectomy.
During breast reconstruction with flap surgery, a plastic surgeon transfers a section of skin, muscle, fat and blood vessels from one part of your body to your chest. The section of tissue is called a flap. The surgeon uses the flap to create a new breast mound. Some people also need a breast implant to get the breast size they want.
Tissue for reconstructing a breast most often comes from the belly. Surgeons also can use tissue from the thighs, back or buttocks. Your surgeon decides which method is best for you based on your body type and your medical and surgical history.
Types of flap surgery
Kinds of tissue flaps commonly used for breast reconstruction include:
- Pedicle flap. A pedicle flap surgery involves moving tissue but keeps most blood vessels in place. The plastic surgeon cuts some of the blood vessels to the tissue for the reconstruction but keeps other blood vessels intact. The surgeon moves the tissue under the skin to the chest area. The surgeon then creates the new breast mound with the tissue.
- Free flap. A free flap surgery involves moving tissue and blood vessels. The plastic surgeon removes the tissue from its blood supply. The surgeon then attaches the tissue to new blood vessels near the chest. Because of the need to reattach blood vessels, free flap surgery most often takes longer than does surgery using a pedicle flap.
The tissue flap used in breast reconstruction with flap surgery needs good blood flow to help it survive. This surgery might not be a good choice if you have a condition that could cause blood flow problems. Examples include diabetes, vascular disease and connective tissue conditions. If you smoke, you need to quit before surgery. Your healthcare team may require that you stop smoking 4 to 6 weeks before your surgery.
TRAM flap
Pedicle TRAM flap
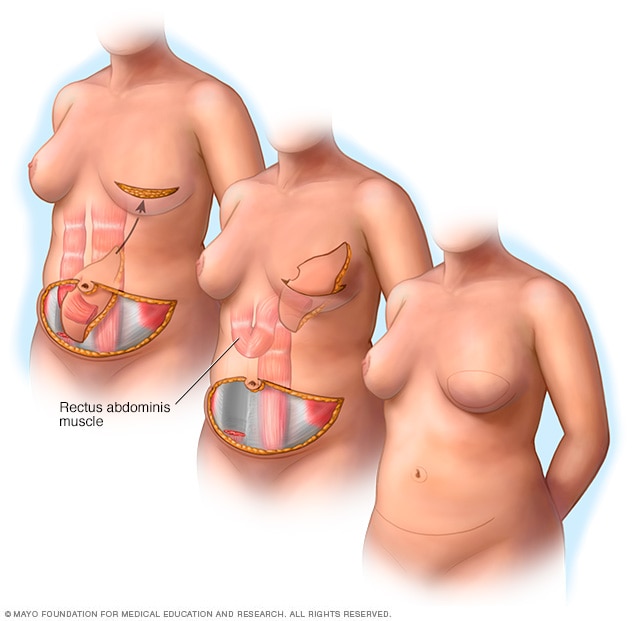
Pedicle TRAM flap
A pedicle transverse rectus abdominis muscle flap procedure uses muscle and tissue from the belly for the new breast. For this surgery, also called a pedicle TRAM flap procedure, the surgeon cuts a section of skin, muscle, fat and blood vessels from the belly. The surgeon then moves the tissue under the skin to the chest. The surgeon uses the tissue to form a new breast mound.
Free TRAM flap
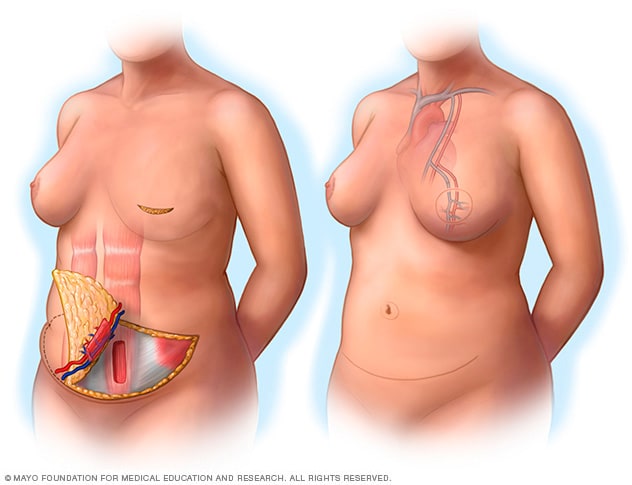
Free TRAM flap
A free transverse rectus abdominis muscle flap procedure uses a section of belly tissue that includes skin, fat and sometimes muscle for the new breast. For this surgery, also called a free TRAM flap procedure, the surgeon removes the tissue from its blood supply and attaches the tissue to blood vessels in the chest area. The surgeon uses the tissue to form a new breast mound.
During transverse rectus abdominis muscle flap surgery, a plastic surgeon removes tissue with muscle from the belly. This procedure also is called TRAM flap surgery. The TRAM flap can be done as a pedicle flap or a free flap.
A pedicle TRAM flap uses the whole rectus muscle. The rectus muscle is one of the major abdominal muscles.
For a muscle-sparing free TRAM flap, a surgeon takes only a part of the rectus abdominis muscle. This may help you keep abdominal strength after surgery.
DIEP flap
DIEP flap
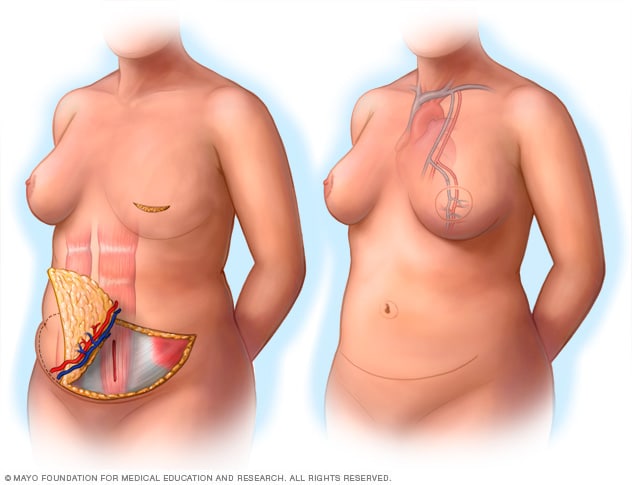
DIEP flap
During a deep inferior epigastric perforator flap procedure, the surgeon removes a section of belly skin, fat and blood vessels for the new breast. This surgery also is called a DIEP flap procedure. The surgeon attaches the tissue to the blood vessels in the chest. The surgeon uses the tissue to create a new breast mound.
Deep inferior epigastric perforator flap surgery, also called DIEP flap surgery, also uses tissue from the belly. It's like TRAM flap surgery, but the surgeon takes only skin and fat from the belly to form the new breast. The surgeon leaves most of the abdominal muscle in place. A plus of this type of breast reconstruction is that it leaves more strength in the abdominal muscles.
The surgeon uses a microscope to help with connecting the tissue flap to blood vessels in the chest.
SEIA flap
Superficial inferior epigastric artery flap surgery also is called SIEA flap surgery. The SIEA flap uses the same belly tissue as the DEIP flap. But it uses blood vessels that aren't as deep within the belly. This is a less invasive surgery. But not everyone has SIEA blood vessels that will work for this type of flap surgery.
TUG flap
Transverse upper gracilis flap surgery, also called TUG flap surgery, uses muscle and fatty tissue from the bottom of the buttocks to the inner thigh.
PAP Flap
Profunda artery perforator flap surgery, also called PAP flap surgery, uses skin and fat from the back of the upper thigh. The benefit of this flap compared to the TUG flap is the surgeon takes no muscle.
Latissimus dorsi flap
Latissimus dorsi flap
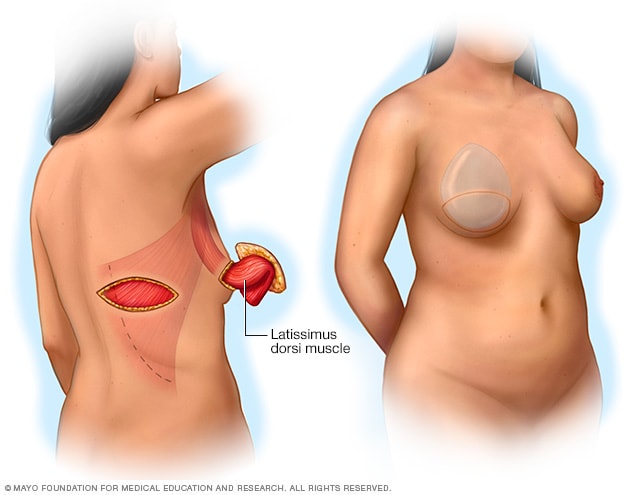
Latissimus dorsi flap
During latissimus dorsi flap surgery, the surgeon takes muscle and tissue from the back. The muscle used in this surgery is called the latissimus dorsi. The surgeon moves the tissue under the skin to its new place and uses it to form a new breast mound.
Latissimus dorsi flap surgery takes skin, fat and muscle from the back. The surgeon transfers it under the skin to the chest. This kind of flap surgery typically takes less skin and fat than other kinds of flaps, so this approach most often uses a breast implant with the flap.
Gluteal flap
A gluteal flap surgery is a free flap procedure that takes tissue from the buttocks and transplants it to the chest area. A gluteal flap may be for people who want tissue reconstruction but who don't have enough extra tissue in their backs or bellies.
After the procedure
After surgery, you may wear a stretchy bandage or support bra to keep swelling down and support the reconstructed breast. You may have a small tube under your skin for a time to drain blood or fluids. Your healthcare professional prescribes medicine to help manage your pain.
You may be tired and sore for several weeks after surgery. Getting back to usual activities takes time. Take it easy during this period.
You might need to restrict your activities. Follow your healthcare team's instructions on what activities are not OK. This may include not doing any overhead lifting or anything that could cause strain.
Contact your plastic surgeon right away if you have worries about your reconstruction.
Nipple reconstruction
Nipple reconstruction
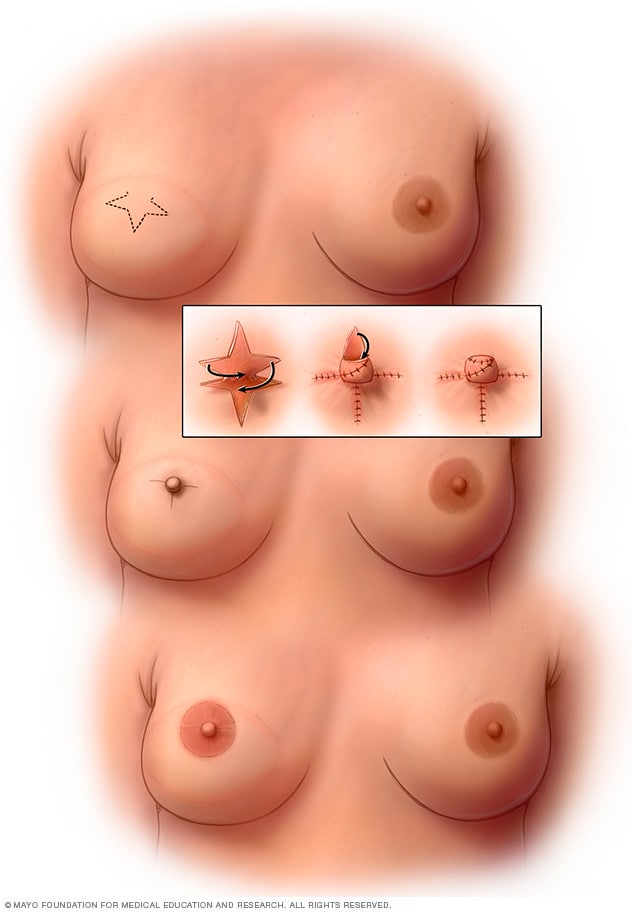
Nipple reconstruction
After the breast has healed from reconstruction or mastectomy, a plastic surgeon can build a new nipple. The surgeon may make a star-shaped cut to form the new nipple. You also may choose to have a tattoo to recreate the circle of skin around the nipple, called the areola.
Breast reconstruction also may involve reconstruction of your nipple, if you choose. Surgery to make a new nipple is called nipple reconstruction. A plastic surgeon does nipple reconstruction most often after you've healed from the flap surgery. After the nipple heals, you may choose to have a tattoo to color the nipple and the circle of skin around it, called the areola.
Future breast cancer screening
If you have only one breast reconstructed, continue with mammograms for breast cancer screening on your other breast. You typically don't need mammograms on breasts that are reconstructed.
Continue to do breast self-exams on both breasts, including your reconstructed breast. Tell your healthcare professional about any changes you find.
Results
The results of breast reconstruction with implants might not be clear right away. It takes time for the tissue on your chest to heal. As your chest heals, you'll likely meet with your surgery team to talk about the results.
The goal of breast reconstruction is to give you the most natural look and feel possible after breast surgery. But breast reconstruction can't make your breast look or feel the same as it did before cancer. It is important to be realistic about what you can expect from breast reconstruction.
What breast reconstruction can do:
- Give your breast a shape.
- Help your breasts look more alike under clothing or in a bathing suit.
- Help you avoid needing to put a breast-shaped form, called a prosthesis, inside your bra.
What breast reconstruction may do:
- Improve how you feel about yourself and your body.
- Take away some of the physical reminders of your cancer.
What breast reconstruction won't do:
- Make you look the same as before your mastectomy.
- Make your reconstructed breast have the same feelings that it had before surgery.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.