Overview
Pituitary tumor

Pituitary tumor
Pituitary tumors are tumors that form in the pituitary gland near the brain. These tumors can cause changes in hormone levels. This illustration shows a smaller tumor, called a microadenoma.
Pituitary tumors are unusual growths that develop in the pituitary gland. This gland is an organ about the size of a pea. It's located behind the nose at the base of the brain. Some of these tumors cause the pituitary gland to make too much of certain hormones that control important body functions. Others can cause the pituitary gland to make too little of those hormones.
Most pituitary tumors are benign. That means they are not cancer. Another name for these noncancerous tumors is pituitary adenomas. Most adenomas stay in the pituitary gland or in the tissue around it, and they grow slowly. They typically don't spread to other parts of the body.
Pituitary tumors can be treated in several ways. The tumor may be removed with surgery. Or its growth may be controlled with medications or radiation therapy. Sometimes, hormone levels are managed with medicine. Your health care provider may suggest a combination of these treatments. In some cases, observation — also called a ''wait-and-see'' approach — may be the right choice.
Types
Types of pituitary adenomas include:
- Functioning. These adenomas make hormones. They cause different symptoms depending on the kind of hormones they make. Functioning pituitary adenomas fall into several categories, including those that make:
- Adrenocorticotropic hormone. This hormone also is known as ACTH. These tumors are sometimes called corticotroph adenomas.
- Growth hormone. These tumors are called somatotroph adenomas.
- Luteinizing hormone and follicle-stimulating hormone. These hormones also are known as gonadotropins. Pituitary tumors that make these hormones are called gonadotroph adenomas.
- Prolactin. These tumors are called prolactinomas or lactotroph adenomas.
- Thyroid-stimulating hormone. These tumors are called thyrotroph adenomas.
- Nonfunctioning. These adenomas don't make hormones. The symptoms they cause are related to the pressure their growth puts on the pituitary gland, nearby nerves and the brain.
- Macroadenomas. These are larger adenomas. They measure about 1 centimeter or more. That's slightly less than a half-inch. They can be functioning or nonfunctioning.
- Microadenomas. These adenomas are smaller. They measure less than 1 centimeter. That's slightly less than a half-inch. They can be functioning or nonfunctioning.
Pituitary tumors are different from pituitary cysts. A cyst is a sac that may be filled with air, fluid or other material. A tumor is an unusual mass of cells that may grow over time. Cysts may form on or near the pituitary gland, but they are not tumors or adenomas.
Products & Services
Symptoms
Not all pituitary tumors cause symptoms. Sometimes these tumors are found during an imaging test, such as an MRI or a CT scan, that is done for another reason. If they don't cause symptoms, pituitary tumors usually don't need treatment.
Pituitary tumor symptoms may be caused by a tumor putting pressure on the brain or on other parts of the body nearby. Symptoms also can be caused by a hormone imbalance. Hormone levels can rise when a pituitary tumor makes too much of one or more hormones. Or a large tumor that disrupts the way the pituitary gland works may cause hormone levels to fall.
Symptoms from tumor pressure
Macroadenomas can put pressure on the pituitary gland, on nerves, on the brain and on other parts of the body nearby. That can cause symptoms such as:
- Headache.
- Eye problems due to pressure on the optic nerve, especially loss of side vision, also called peripheral vision, and double vision.
- Pain in the face, sometimes including sinus pain or ear pain.
- Drooping eyelid.
- Seizures.
- Nausea and vomiting.
Symptoms from hormone changes
Cushing syndrome
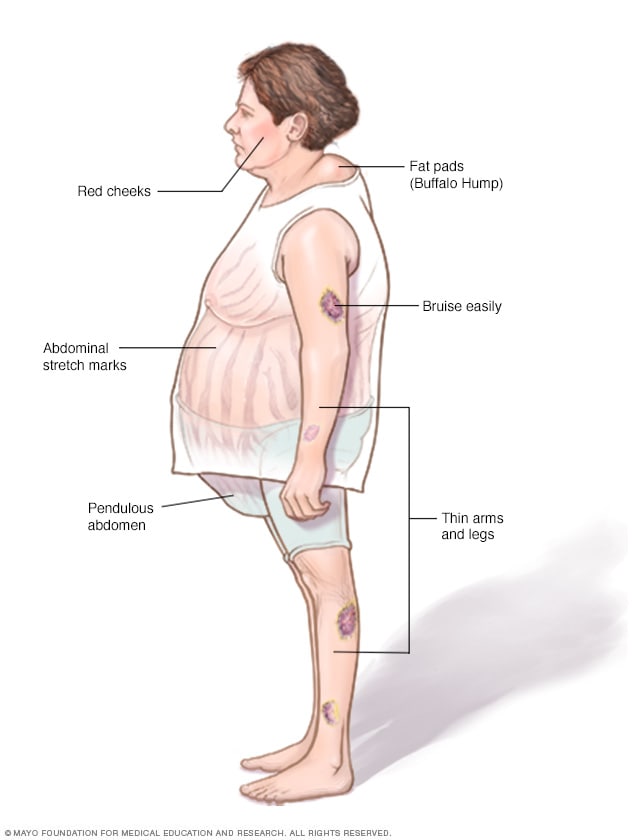
Cushing syndrome
Without treatment, Cushing syndrome can cause facial roundness, weight gain around the middle body and upper back, thinning of the arms and legs, easy bruising, and stretch marks.
Person with acromegaly

Person with acromegaly
Symptoms of acromegaly include an enlarged face and hands. Changes to the face may cause the brow bone and lower jaw to jut out, and the nose and lips to get larger.
Low amounts of hormones
Macroadenomas can limit the pituitary gland's ability to make hormones. When that happens, symptoms may include:
- Tiredness or weakness.
- Lack of energy.
- Sexual problems, such as problems with erections and less interest in sex.
- Changes in menstrual cycles.
- Nausea.
- Feeling cold.
- Losing or gaining weight without trying.
High amounts of hormones
Functioning pituitary adenomas typically make a large amount of one hormone. That exposes the body to high levels of that hormone. Rarely, a pituitary adenoma may make more than one hormone. The following types of functioning pituitary adenomas cause different symptoms depending on the hormones they make.
Pituitary tumors that make adrenocorticotropic hormone
Pituitary tumors that make adrenocorticotropic hormone are called corticotroph adenomas. Adrenocorticotropic hormone, also called ACTH, causes the adrenal glands to make the hormone cortisol. ACTH tumors trigger the adrenal glands to make too much cortisol. This causes a condition called Cushing disease. Cushing disease is one cause of Cushing syndrome.
Cushing disease symptoms include:
- Weight gain and fatty tissue deposits around the midsection and upper back.
- Rounded face.
- Stretch marks.
- Thin skin that bruises easily.
- Thinning of the arms and legs with muscle weakness.
- Thicker or more visible body hair.
- Slow healing of cuts, insect bites and infections.
- Areas of darkened skin.
- Acne.
- Changes in menstrual cycles.
- Sexual problems, including problems with erections and less interest in sex.
Pituitary tumors that make growth hormone
Pituitary tumors that make growth hormone also are called growth hormone-secreting tumors or somatotroph adenomas. Too much growth hormone leads to a condition known as acromegaly. Acromegaly can cause:
- Changes in facial features, including larger lips, nose and tongue; longer lower jaw; and wide spaces between teeth.
- Growth of hands and feet.
- Thicker skin.
- More sweating and body odor.
- Joint pain.
- A deeper voice.
Children and teens who have too much growth hormone might also grow faster or taller than usual. This condition is called gigantism.
Pituitary tumors that make luteinizing hormone and follicle-stimulating hormone
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are also known as gonadotropins. Pituitary tumors that make these hormones are called gonadotroph adenomas.
It's uncommon for these adenomas to make too many hormones that then trigger symptoms. Instead, symptoms from these adenomas usually are due to tumor pressure. If symptoms do happen because of too much LH and FSH, they affect women and men differently.
Symptoms in women may include:
- Change in menstrual cycles.
- Fertility problems.
- Enlargement of and pain in the ovaries caused by a condition called ovarian hyperstimulation syndrome.
Symptoms in men may include:
- Enlarged testicles.
- Higher levels of testosterone.
Pituitary tumors that make prolactin
These adenomas are called prolactinomas. Too much of the hormone prolactin can lead to a decrease in the body's levels of sex hormones — estrogen and testosterone. Too much prolactin affects men and women differently.
In women, too much prolactin might cause:
- Irregular menstrual cycles.
- Lack of menstrual cycles.
- Milky discharge from the breasts.
- Breast tenderness.
- Problems with fertility.
- Less interest in sex.
In men, too much prolactin can cause a condition called male hypogonadism. Symptoms might include:
- Problems with erections.
- Less interest in sex.
- Breast growth.
- Problems with fertility.
- Less body and facial hair.
Pituitary tumors that make thyroid-stimulating hormone
Pituitary tumors that make thyroid-stimulating hormone are called thyrotroph adenomas. They also may be referred to as thyroid-stimulating hormone-secreting tumors. They cause the thyroid gland to make too much of the hormone thyroxine, also called T-4. That leads to a condition called hyperthyroidism, also known as overactive thyroid disease. Hyperthyroidism can speed up the body's metabolism causing many symptoms. Some of the most common include:
- Weight loss.
- Rapid or irregular heartbeat.
- Nervousness, anxiety or irritability.
- Frequent bowel movements.
- Sweating.
- Tremor.
- Sleep problems.
When to see a doctor
If you develop symptoms that might be associated with a pituitary tumor, see your health care provider. Treatment for pituitary tumors often can bring hormones back to a healthy level and ease symptoms.
Although rare, some pituitary tumors are hereditary. That means they run in families. In particular, the hereditary disorder multiple endocrine neoplasia, type 1 (MEN 1) can cause pituitary tumors. If MEN 1 runs in your family, talk to your health care provider about tests that may help find a pituitary tumor early.
Causes
Pituitary gland and hypothalamus
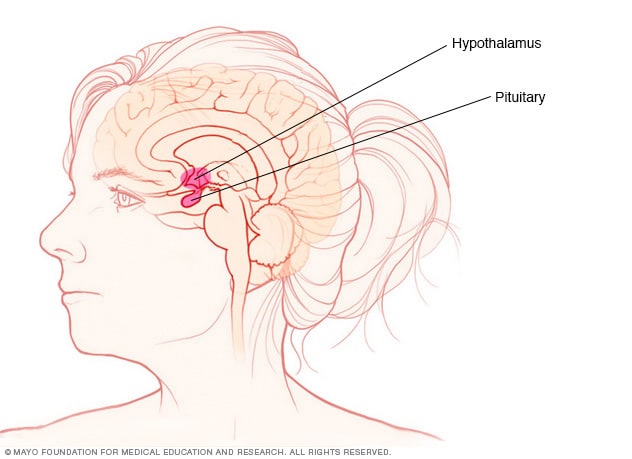
Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus are in the brain. They make hormones that control many important functions in the body.
The pituitary gland is a small organ about the size of a pea. It's located behind the nose at the base of the brain. Despite its small size, the pituitary gland has an effect on nearly every part of the body. The hormones it makes control important body functions, such as growth, blood pressure and reproduction.
The cause of uncontrolled cell growth in the pituitary gland, which creates a tumor, remains unknown. In rare cases, pituitary tumors can be caused by genes you've inherited. But most have no clear hereditary cause. Still, scientists think that changes in genes may play an important role in how pituitary tumors develop.
Risk factors
Most people who get pituitary tumors don't have any factors that put them at higher risk of developing these tumors. Environment and lifestyle choices don't seem to have an effect on a person's risk of pituitary tumors.
Although genetics seems to play a role, most people who have pituitary tumors don't have a family history of them.
The only known risk factors are several rare hereditary conditions that raise the risk of many health problems, including pituitary tumors. These conditions include:
- Multiple endocrine neoplasia, type 1, also called MEN 1.
- Multiple endocrine neoplasia, type 4, also called MEN 4.
- Carney complex.
- McCune-Albright syndrome.
Complications
Pituitary tumors usually don't spread to other parts of the body. They can affect a person's health, though. Pituitary tumors may cause:
- Problems with eyesight, including vision loss.
- High blood pressure.
- High blood sugar.
- Bone loss.
- Heart problems.
- Problems with thinking and memory.
Seizures
If a pituitary tumor presses on part of the brain called the medial temporal lobe, it may lead to a seizure. This type of seizure is known as a focal seizure with impaired awareness. These seizures involve a change in or loss of consciousness or awareness. If you have one of these seizures, you may seem to be awake. But you stare into space and don't respond as you typically would to the environment around you. You may not remember the seizure after it happens.
Permanent low hormone levels
Having a pituitary tumor or having one removed with surgery may permanently change your body's hormone supply. As a result, you may need hormone replacement therapy for the rest of your life.
Pituitary apoplexy
A rare but potentially serious complication of a pituitary tumor is pituitary apoplexy. This happens when there is sudden bleeding into the tumor. Symptoms include:
- A severe headache, likely worse than you've ever had before.
- Problems with your eyesight, including double vision or loss of vision in one or both eyes.
- Nausea and vomiting.
- Confusion or other reduced mental function.
Pituitary apoplexy requires emergency treatment. The treatment usually includes taking corticosteroid medicine to ease swelling around the tumor. You also may need surgery to remove the tumor.