Overview
What is thyroid cancer? A Mayo Clinic expert explains
Learn more about thyroid cancer from endocrinologist Mabel Ryder, M.D.
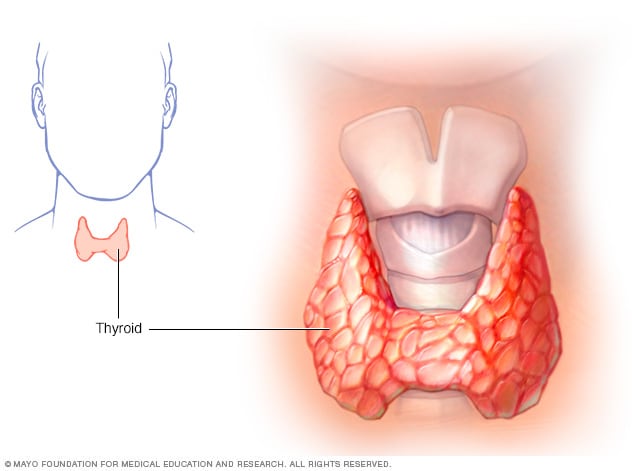
I'm Dr. Mabel Ryder, an endocrinologist at Mayo Clinic. In this video, we'll cover the basics of thyroid cancer: What is it? Who gets it? The symptoms. Diagnosis and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available. What is the thyroid? This is a butterfly shaped gland that sits at the base of your neck. It's an important gland responsible for producing hormones that control a lot of vital functions in your body, such as your heart and your heart rate, your blood pressure, your body temperature, and your weight. When thyroid cells mutate, changes to their DNA cause them to grow and multiply. Where healthy cells typically die, these abnormal cells grow and grow and eventually form a tumor. Sometimes these cells invade nearby tissue, and can spread or metastasize to other parts of the body. There are several different kinds of thyroid cancer. Some grow slowly. Others can be more aggressive. Because we're able to detect small thyroid cancers with new technology, the rate of thyroid cancer incidence has gone up. However, most cancers are very treatable and the prognosis for most patients with thyroid cancer is excellent.
There are other things that can increase your chances of developing thyroid cancer. Women are three times more likely to develop thyroid cancer. And exposure to high levels of radiation, for instance, radiation therapy to the head or neck for other cancers, can increase your risk. Certain hereditary genetic syndromes may also play a role. Different types of thyroid cancer are more likely to affect different age groups. Papillary thyroid cancer is the most common form of thyroid cancer. And although it can occur at any age, it generally affects people ages 30 to 50. Follicular thyroid cancer usually affects people older than age 50. Anaplastic thyroid cancer is a very rare type of cancer that typically occurs in adults 60 and older. And medullary thyroid cancer. Although uncommon, up to 30 percent of patients with medullary thyroid cancer are associated with genetic syndromes that can increase your risk for other tumors as well.
Typically, thyroid cancer doesn't trigger any signs or symptoms in its early stages. As it grows, you may notice a lump that can be felt through the skin in your neck. You may notice changes to your voice, including hoarseness of your voice, or difficulty swallowing. Some may develop pain in their neck or throat. Or you may develop swollen lymph nodes in your neck. If you're experiencing any of these issues and are concerned, make an appointment with your doctor.
Most often, diagnosing thyroid cancer starts with the physical exam. Your doctor will feel for physical changes in your neck and the thyroid. This usually is followed by blood tests and ultrasound imaging. Armed with this information, doctors may decide to do a biopsy to remove a small sample of tissue from your thyroid. In some cases, genetic testing may be done to help determine any associated hereditary causes. If diagnosed with thyroid cancer, several other tests may be done to help your doctor determine whether your cancer has spread beyond the thyroid and outside of the neck. These tests may include blood tests to check tumor markers and imaging tests, such as CT scans, MRI, or nuclear imaging tests, such as a radioiodine whole-body scan.
Fortunately, most thyroid cancers can be beaten with treatments. Very small cancers - under 1 centimeter - have a low risk of growing or spreading and, thus, might not need treatment right away. Instead, your doctor may recommend observation with blood tests, an ultrasound, and a physical exam once or twice per year. In many people, this small cancer - under 1 centimeter - might never grow and may never require surgery. In cases where further treatment is necessary, surgery is common. Depending on your cancer, your doctor may remove just a portion of the thyroid - a procedure known as thyroidectomy. Or your doctor may remove all of the thyroid. Other treatments may include thyroid hormone therapy, alcohol ablation, radioactive iodine, targeted drug therapy, external radiation therapy, and chemotherapy, in some. Ultimately, what your treatment looks like will depend on the stage of your cancer and the type of thyroid cancer you have.
If you've been diagnosed with thyroid cancer, you might feel as if you aren't sure what to do next. And that's normal, everyone eventually find their own way of coping with a cancer diagnosis. But until you find what works for you, try the following. Learn all you can to help you make decisions about your care. Connect with other survivors. Talking to people who share your situation can be incredibly helpful. And control what you can about your health. Take steps to keep your body healthy during and after treatment. Eat a healthy diet full of a variety of fruits and vegetables. Get enough rest. And try to incorporate physical activity when you can. Being diagnosed with cancer can be frightening, but take comfort in the fact that most cases of this cancer are treatable. If you'd like to learn even more about thyroid cancer, watch our other related videos or visit mayoclinic.org. We wish you well.
Thyroid cancer

Thyroid cancer
Thyroid cancer occurs in the cells of the thyroid.
Thyroid cancer is a growth of cells that starts in the thyroid. The thyroid is a butterfly-shaped gland located at the base of the neck, just below the Adam's apple. The thyroid produces hormones that regulate heart rate, blood pressure, body temperature and weight.
Thyroid cancer might not cause any symptoms at first. But as it grows, it can cause signs and symptoms, such as swelling in your neck, voice changes and difficulty swallowing.
Several types of thyroid cancer exist. Most types grow slowly, though some types can be very aggressive. Most thyroid cancers can be cured with treatment.
Thyroid cancer rates seem to be increasing. The increase may be caused by improved imaging technology that allows health care providers to find small thyroid cancers on CT and MRI scans done for other conditions (incidental thyroid cancers). Thyroid cancers found in this way are usually small cancers that respond well to treatments.
Products & Services
Symptoms
Thyroid gland
Thyroid gland
The thyroid gland sits at the base of the neck.
Most thyroid cancers don't cause any signs or symptoms early in the disease. As thyroid cancer grows, it may cause:
- A lump (nodule) that can be felt through the skin on your neck
- A feeling that close-fitting shirt collars are becoming too tight
- Changes to your voice, including increasing hoarseness
- Difficulty swallowing
- Swollen lymph nodes in your neck
- Pain in your neck and throat
When to see a doctor
If you experience any signs or symptoms that worry you, make an appointment with your health care provider.
Causes
Thyroid cancer happens when cells in the thyroid develop changes in their DNA. A cell's DNA contains the instructions that tell the cell what to do. The changes, which doctors call mutations, tell the cells to grow and multiply rapidly. The cells go on living when healthy cells would naturally die. The accumulating cells form a mass called a tumor.
The tumor can grow to invade nearby tissue and can spread (metastasize) to the lymph nodes in the neck. Sometimes the cancer cells can spread beyond the neck to the lungs, bones and other parts of the body.
For most thyroid cancers, it's not clear what causes the DNA changes that cause the cancer.
Types of thyroid cancer
Thyroid cancer is classified into types based on the kinds of cells found in the tumor. Your type is determined when a sample of tissue from your cancer is examined under a microscope. The type of thyroid cancer is considered in determining your treatment and prognosis.
Types of thyroid cancer include:
- Differentiated thyroid cancers. This broad category includes types of thyroid cancer that start in the cells that produce and store thyroid hormones. These cells are called follicular cells. Differentiated thyroid cancers cells appear similar to healthy cells when viewed under a microscope.
- Papillary thyroid cancer. This is the most common type of thyroid cancer. It can happen at any age, but it most often affects people ages 30 to 50. Most papillary thyroid cancers are small and respond well to treatment, even if the cancer cells spread to the lymph nodes in the neck. A small portion of papillary thyroid cancers are aggressive and may grow to involve structures in the neck or spread to other areas of the body.
- Follicular thyroid cancer. This rare type of thyroid cancer usually affects people older than 50. Follicular thyroid cancer cells don't often spread to the lymph nodes in the neck. But some large and aggressive cancers may spread to other parts of the body. Follicular thyroid cancer most often spreads to the lungs and bones.
- Hurthle cell thyroid cancer. This rare type of thyroid cancer was once considered a type of follicular thyroid cancer. Now it is considered its own type because the cancer cells behave differently and respond to different treatments. Hurthle cell thyroid cancers are aggressive and can grow to involve structures in the neck and spread to other parts of the body.
- Poorly differentiated thyroid cancer. This rare type of thyroid cancer is more aggressive than other differentiated thyroid cancers and often doesn't respond to the usual treatments.
- Anaplastic thyroid cancer. This rare type of thyroid cancer grows quickly and can be difficult to treat. However, treatments can help slow the progression of the disease. Anaplastic thyroid cancer tends to occur in people older than 60. It can cause severe signs and symptoms, such as neck swelling that worsens very quickly and may lead to difficulty breathing and swallowing.
- Medullary thyroid cancer. This rare type of thyroid cancer begins in thyroid cells called C cells, which produce the hormone calcitonin. Elevated levels of calcitonin in the blood can indicate medullary thyroid cancer at a very early stage. Some medullary thyroid cancers are caused by a gene called RET that's passed from parents to children. Changes in the RET gene can cause familial medullary thyroid cancer and multiple endocrine neoplasia, type 2. Familial medullary thyroid cancer increases the risk of thyroid cancer. Multiple endocrine neoplasia, type 2, increases the risk of thyroid cancer, adrenal gland cancer and other types of cancers.
- Other rare types. Other very rare types of cancer can start in the thyroid. These include thyroid lymphoma, which begins in the immune system cells of the thyroid, and thyroid sarcoma, which begins in the connective tissue cells of the thyroid.
Risk factors
Factors that may increase the risk of thyroid cancer include:
- Female sex. Thyroid cancer occurs more often in women than in men. Experts think it may be related to the hormone estrogen. People who are assigned female sex at birth generally have higher levels of estrogen in their bodies.
- Exposure to high levels of radiation. Radiation therapy treatments to the head and neck increase the risk of thyroid cancer.
- Certain inherited genetic syndromes. Genetic syndromes that increase the risk of thyroid cancer include familial medullary thyroid cancer, multiple endocrine neoplasia, Cowden syndrome and familial adenomatous polyposis. Types of thyroid cancer that sometimes run in families include medullary thyroid cancer and papillary thyroid cancer.
Complications
Thyroid cancer that comes back
Thyroid cancer can return despite successful treatment, and it can even come back if you've had your thyroid removed. This could happen if cancer cells spread beyond the thyroid before it's removed.
Most thyroid cancers aren't likely to recur, including the most common types of thyroid cancer — papillary thyroid cancer and follicular thyroid cancer. Your health care provider can tell you if your cancer has an increased risk of recurring based on the particulars of your cancer.
Recurrence is more likely if your cancer is aggressive or if it grows beyond your thyroid. When thyroid cancer recurrence happens, it's usually found in the first five years after your initial diagnosis.
Thyroid cancer that comes back still has a good prognosis. It's often treatable, and most people will have successful treatment.
Thyroid cancer may recur in:
- Lymph nodes in the neck
- Small pieces of thyroid tissue left behind during surgery
- Other areas of the body, such as the lungs and bones
Your health care provider may recommend periodic blood tests or thyroid scans to check for signs that your cancer has returned. At these appointments, your provider may ask if you've experienced any signs and symptoms of thyroid cancer recurrence, such as:
- Neck pain
- A lump in the neck
- Trouble swallowing
- Voice changes, such as hoarseness
Thyroid cancer that spreads (metastasizes)
Thyroid cancer sometimes spreads to nearby lymph nodes or to other parts of the body. The cancer cells that spread might be found when you're first diagnosed or they might be found after treatment. The great majority of thyroid cancers don't ever spread.
When thyroid cancer spreads, it most often travels to:
- Lymph nodes in the neck
- Lungs
- Bones
- Brain
- Liver
- Skin
Thyroid cancer that spreads might be detected on imaging tests, such as CT and MRI, when you're first diagnosed with thyroid cancer. After successful treatment, your health care provider might recommend follow-up appointments to look for signs that your thyroid cancer has spread. These appointments might include nuclear imaging scans that use a radioactive form of iodine and a special camera to detect thyroid cancer cells.
Prevention
Doctors aren't sure what causes the gene changes that lead to most thyroid cancers, so there's no way to prevent thyroid cancer in people who have an average risk of the disease.
Prevention for people with a high risk
Adults and children with an inherited gene that increases the risk of medullary thyroid cancer may consider thyroid surgery to prevent cancer (prophylactic thyroidectomy). Discuss your options with a genetic counselor who can explain your risk of thyroid cancer and your treatment options.
Prevention for people near nuclear power plants
A medication that blocks the effects of radiation on the thyroid is sometimes provided to people living near nuclear power plants in the United States. The medication (potassium iodide) could be used in the unlikely event of a nuclear reactor accident. If you live within 10 miles of a nuclear power plant and are concerned about safety precautions, contact your state or local emergency management department for more information.
Jan. 05, 2024