Overview
Thoracic aortic aneurysm

Thoracic aortic aneurysm
A thoracic aortic aneurysm is a weakened area in the upper part of the aorta — the major blood vessel that feeds blood to the body. Aneurysms can develop anywhere in the aorta.
A thoracic aortic aneurysm is a weakened area in the body's main artery in the chest. The body's main artery is called the aorta. When the aortic wall is weak, the artery may widen. When the vessel is significantly widened, it's called an aneurysm.
A thoracic aortic aneurysm also is called a thoracic aneurysm.
Treatment of a thoracic aortic aneurysm may vary from regular health checkups to emergency surgery. The type of treatment depends on the cause, size and growth rate of the thoracic aortic aneurysm.
Complications of a thoracic aortic aneurysm include rupture of the aorta or a life-threatening tear between the layers of the aorta's wall. The tear is called an aortic dissection. Rupture or dissection can lead to sudden death.
Thoracic aortic aneurysms are less common than aneurysms that form in the lower part of the aorta, called abdominal aortic aneurysms.
Symptoms
Thoracic aortic aneurysms often grow slowly. There are usually no symptoms, making them difficult to detect. Many start small and stay small. Others grow bigger over time. How quickly a thoracic aortic aneurysm may grow is difficult to predict.
As a thoracic aortic aneurysm grows, symptoms may include:
- Back pain.
- Cough.
- Weak, scratchy voice.
- Shortness of breath.
- Tenderness or pain in the chest.
Symptoms that a thoracic aortic aneurysm has ruptured or dissected include:
- Sharp, sudden pain in the upper back that spreads downward.
- Pain in the chest, jaw, neck or arms.
- Difficulty breathing.
- Low blood pressure.
- Loss of consciousness.
- Shortness of breath.
- Trouble swallowing.
Some aneurysms may never rupture or lead to dissection.
When to see a doctor
Most people with aortic aneurysms don't have symptoms unless a dissection or rupture occurs. An aortic dissection or aneurysm rupture is a medical emergency. Call 911 or your local emergency number for immediate help.
Causes
Aortic aneurysms can develop anywhere in the body's main artery, called the aorta. The aorta runs from the heart through the chest and belly area. When an aneurysm occurs in the chest, it's called a thoracic aortic aneurysm.
If an aneurysm forms between the upper and lower parts of the aorta, it's called a thoracoabdominal aneurysm.
A thoracic aneurysm may be round or tube-shaped.
Aneurysms can occur anywhere in the thoracic aorta, including near the heart, in the aortic arch and in the lower part of the thoracic aorta.
Causes of thoracic aortic aneurysms may include:
- Hardening of the arteries, called atherosclerosis. Plaque buildup on the artery walls causes the arteries to become less flexible. Additional pressure can cause the arteries to weaken and widen. High blood pressure and high cholesterol increase the risk of atherosclerosis. This is more common in older people.
-
Genetic conditions. Aortic aneurysms in younger people often have a genetic cause. Marfan syndrome, a genetic condition that affects the connective tissue in the body, may cause weakness in the wall of the aorta.
Other genetic conditions linked to aortic aneurysm and dissection and rupture include vascular Ehlers-Danlos, Loeys-Dietz and Turner syndromes.
- Blood vessel inflammation. Conditions that involve blood vessel inflammation, such as giant cell arteritis and Takayasu arteritis, are associated with thoracic aortic aneurysms.
- Irregular aortic valve. The aortic valve is between the lower left heart chamber and the aorta. People who are born with an aortic valve that has only two flaps instead of three have an increased risk of a thoracic aneurysm.
- Untreated infection. Though rare, it's possible to develop a thoracic aortic aneurysm if you've had an untreated infection, such as syphilis or salmonella.
- Traumatic injury. Rarely, some people who are injured in falls or motor vehicle crashes develop thoracic aortic aneurysms.
Aortic emergencies
Aortic aneurysm and aortic dissection
Aortic aneurysm and aortic dissection
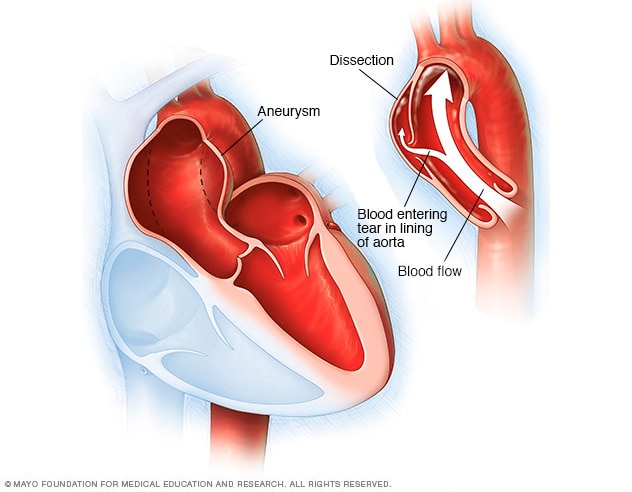
An aortic aneurysm occurs when a weak spot in the wall of the aorta begins to bulge, as shown in the image on the left. An aneurysm can occur anywhere in the aorta. Having an aortic aneurysm increases the risk of a tear in the aortic lining, called a dissection, as shown in the image on the right.
In aortic dissection, a tear occurs in the wall of the aorta. This causes bleeding into and along the aortic wall. Sometimes the bleeding moves completely outside the aorta. When this happens, it's called an aortic rupture.
An aortic dissection is a potentially life-threatening emergency, depending on where in the aorta it occurs. It's important to treat an aortic aneurysm to try to prevent dissection. If dissection occurs, people can still be treated with surgery. However, they typically have a higher risk of complications.
Risk factors
Thoracic aortic aneurysm risk factors include:
- Age. Growing older increases the risk of aortic aneurysms. Thoracic aortic aneurysms occur most often in people age 65 and older.
- Tobacco use. Smoking and using tobacco greatly increases the risk of an aortic aneurysm.
- High blood pressure. Increased blood pressure damages the blood vessels in the body, raising the risk of an aneurysm.
- Buildup of plaques in the arteries. The buildup of fat and other substances in the blood can damage the lining of a blood vessel, increasing the risk of an aneurysm. This is a more common risk in older people.
- Family history. Having a parent, brother, sister or child with an aortic aneurysm increases the risk of an aortic aneurysm and rupture. You may develop aneurysms at a younger age.
- Genetic conditions. If you have Marfan syndrome or a related condition, such as Loeys-Dietz syndrome or vascular Ehlers-Danlos syndrome, you have a significantly higher risk of a thoracic aortic aneurysm. The risk also is increased for an aortic or other blood vessel dissection or rupture.
- Bicuspid aortic valve. Having an aortic valve with two cusps instead of three increases the risk of aortic aneurysm.
Complications
Tears in the wall of the aorta and rupture of the aorta are the main complications of thoracic aortic aneurysm. However, some small and slow-growing aneurysms may never rupture. In general, the larger the aneurysm, the greater the risk of rupture.
Complications of a thoracic aortic aneurysm and rupture can include:
- Life-threatening bleeding inside the body. This is called internal bleeding. Emergency surgery is required to try to prevent death.
- Blood clots. Small blood clots can develop in the area of the aortic aneurysm. If a blood clot breaks loose from the inside wall of an aneurysm, it can block a blood vessel elsewhere in the body. This can possibly cause serious complications.
- Stroke. Signs and symptoms of stroke include weakness of or an inability to move one side of the body. It may be difficult to speak.
Prevention
Keeping the blood vessels as healthy as possible is important in preventing an aneurysm. A health care provider may recommend these heart-healthy strategies:
- Don't smoke or use tobacco products.
- Keep blood pressure and cholesterol levels under control.
- Get regular exercise.
- Reduce cholesterol and fat in the diet.
There are no medicines to prevent an aortic aneurysm. However, medicines may be used to treat high blood pressure, high cholesterol and other conditions linked to aneurysm. Proper management of such conditions may lower the risk of thoracic aortic aneurysm complications.
Screening and genetic testing
Conditions that cause a thoracic aortic aneurysm may run in families. A health care provider may recommend screening if a first-degree relative — such as a parent, brother, sister, son or daughter — has a genetic disease such as Marfan syndrome or another condition linked to thoracic aortic aneurysms.
Screening means you have regular imaging tests, usually an echocardiogram, to check for an aneurysm. If an ultrasound of the heart shows an enlarged aorta or an aneurysm, another imaging test is usually done within 6 to 12 months to make sure it hasn't grown.
Genetic testing also may be recommended if you have a family history of aortic aneurysms, particularly if you're considering pregnancy.